PCOS
Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disorder (PCOD) are two conditions that are often confused due to their similar names and symptoms. However, they are distinct medical conditions with their own set of characteristics and implications. In this blog post, we will discuss thoroughly about both PCOD and PCOS to shed light on these often-misunderstood conditions.
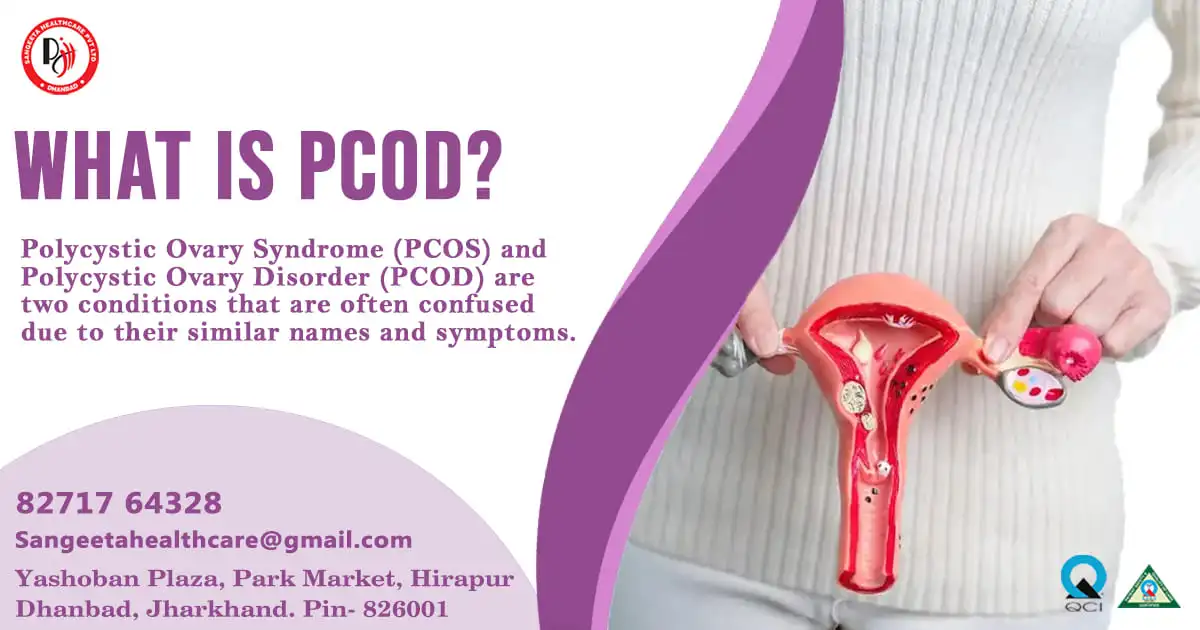
What is PCOD?
Polycystic Ovary Disorder (PCOD), also known as Polycystic Ovarian Syndrome (PCOS), is a hormonal disorder characterized by the presence of multiple small cysts on the ovaries. However, not all individuals diagnosed with PCOD necessarily have cysts. PCOD is primarily a reproductive disorder, often resulting in irregular menstrual cycles and difficulties in conceiving.
Key Features of PCOD:
- Menstrual Irregularities: Women with PCOD frequently experience irregular menstrual cycles, including prolonged periods, scanty bleeding, or even absence of menstruation.
- Hormonal Imbalance: PCOD is associated with hormonal imbalances, particularly elevated levels of androgens (male hormones) such as testosterone.
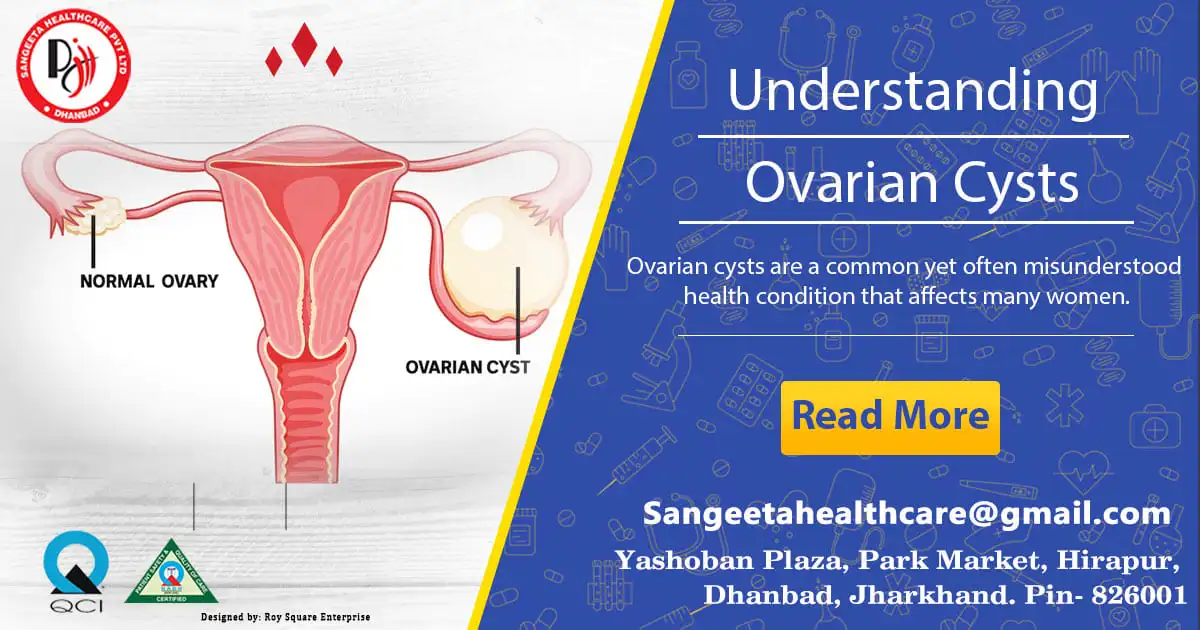
- Ovarian Cysts: While the name suggests the presence of cysts, not all individuals with PCOD develop ovarian cysts. These cysts are tiny, fluid-filled pouches that grow on the ovaries.
Metabolic Issues: PCOD is often linked with metabolic disturbances such as insulin resistance, which can lead to weight gain, type 2 diabetes, and other health complications
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a broader condition that encompasses not only ovarian cysts but also a range of other symptoms related to hormonal imbalance. One of the most prevalent endocrine conditions affecting women who are fertile is PCOS.
Key Features of PCOS:
- Menstrual Irregularities: Similar to PCOD, women with PCOS may experience irregular menstrual cycles, often characterized by oligo menorrhea (infrequent periods) or amenorrhea (absence of menstruation).
- Hormonal Imbalance: PCOS is characterized by high levels of androgens, insulin resistance, and abnormalities in other hormones such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- Ovarian Cysts: The presence of ovarian cysts is common in PCOS, but they are not a prerequisite for diagnosis. These cysts are typically small and numerous, giving the ovaries a characteristic “polycystic” appearance on ultrasound.
- Metabolic Issues: Insulin resistance and metabolic syndrome are common in individuals with PCOS, increasing the risk of obesity, type 2 diabetes, cardiovascular disease, and other metabolic complications.
Is PCOD and PCOS same?
PCOD (Polycystic Ovary Disorder) and PCOS (Polycystic Ovary Syndrome) are related conditions, but they are not exactly the same. They share some similarities but also have differences that set them apart. Here’s a breakdown:
Similarities:
- Ovarian Cysts: Both PCOD and PCOS involve the presence of ovarian cysts, although they may vary in number and size.
- Hormonal Imbalance: Both conditions are characterized by hormonal imbalances, particularly elevated levels of androgens (male hormones) such as testosterone, and irregularities in other hormones like LH and FSH.
- Menstrual Irregularities: Women with PCOD and PCOS often experience irregular menstrual cycles, which can manifest as prolonged periods, scanty bleeding, or absence of menstruation altogether.
While PCOD and PCOS share similarities, they are not the same condition. PCOS is a broader syndrome with a wider range of symptoms and associated health risks, including metabolic complications. PCOD primarily focuses on ovarian and menstrual irregularities. It’s important to consult with a healthcare professional for proper diagnosis and management tailored to individual needs, whether you suspect PCOD or PCOS.
Recognize what is the Difference between PCOD and PCOS:
- Diagnostic Criteria: PCOD is primarily diagnosed based on ultrasound findings of ovarian cysts and clinical symptoms, whereas PCOS diagnosis involves a broader set of criteria, including ovarian cysts, hormonal imbalances, and metabolic abnormalities.
- Scope of Symptoms: PCOS encompasses a wider range of symptoms beyond ovarian cysts, including insulin resistance, obesity, hirsutism (excessive hair growth), acne, and infertility, whereas PCOD primarily focuses on ovarian and menstrual irregularities.
- Severity of Condition: PCOS is generally considered a more severe condition due to its broader spectrum of symptoms and associated metabolic complications compared to PCOD.
- Treatment Approach: While the management of both conditions involves lifestyle modifications, hormonal therapy, and fertility treatments, the approach to managing PCOS may also include medications to address insulin resistance and metabolic issues.
Understanding the differences between PCOD and PCOS can help individuals navigate their healthcare journey more effectively, leading to better management of their symptoms and improved quality of life.
In summary, while PCOD and PCOS share similarities such as menstrual irregularities and ovarian cysts, they are distinct conditions with differences in diagnostic criteria, symptomatology, and associated health risks. Understanding these differences is crucial for accurate diagnosis and appropriate management strategies tailored to each individual’s needs. If you suspect you may have PCOD or PCOS, consult with a healthcare professional for proper evaluation and personalized treatment.
Difference between PCOS and PCOD symptoms
Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disorder (PCOD) share some common symptoms, but they also have distinct characteristics. Here’s a breakdown of the differences in symptoms between PCOS and PCOD:
PCOS Symptoms:
- Irregular Menstrual Cycles:
- Women with PCOS often experience irregular menstrual cycles, which may include oligomenorrhea (infrequent periods) or amenorrhea (absence of menstruation).
- Ovarian Cysts:
- PCOS is characterized by the presence of multiple small ovarian cysts. These cysts are typically numerous and give the ovaries a characteristic “polycystic” appearance on ultrasound.
- Hormonal Imbalances:
- Elevated levels of androgens (male hormones), such as testosterone, are common in women with PCOS. This hormonal imbalance can lead to symptoms such as hirsutism (excessive hair growth), acne, and male-pattern baldness.
- Insulin Resistance:
- Many women with PCOS have insulin resistance, which impairs the body’s ability to use insulin effectively. Insulin resistance can lead to weight gain, especially around the abdomen, and increases the risk of type 2 diabetes and cardiovascular disease.
- Metabolic Disturbances:
- PCOS is associated with metabolic disturbances, including dyslipidemia (abnormal lipid levels), hypertension (high blood pressure), and an increased risk of metabolic syndrome.
PCOD Symptoms:
- Menstrual Irregularities:
- Similar to PCOS, women with PCOD often experience irregular menstrual cycles. This can manifest as prolonged periods, scanty bleeding, or unpredictable menstruation.
- Ovarian Cysts:
- PCOD is characterized by the presence of multiple small cysts on the ovaries. However, not all women with PCOD develop ovarian cysts, and the presence of cysts is not necessary for diagnosis.
- Hormonal Imbalances:
- Hormonal imbalances are common in PCOD, including elevated levels of androgens such as testosterone. These hormonal disturbances can lead to symptoms similar to those seen in PCOS, such as hirsutism and acne.
- Metabolic Issues:
- While PCOD primarily affects the reproductive system, it is also associated with metabolic issues such as insulin resistance and an increased risk of type 2 diabetes and cardiovascular disease.
Key Differences:
- PCOS is a syndrome that encompasses ovarian cysts, hormonal imbalances, and metabolic disturbances, whereas PCOD primarily focuses on ovarian and menstrual irregularities.
- Insulin resistance and metabolic syndrome are more commonly associated with PCOS, while PCOD may primarily present with ovarian and menstrual symptoms.
- PCOS tends to be associated with more severe hormonal and metabolic disturbances, whereas PCOD may have a milder presentation in some cases.
In summary, while PCOS and PCOD share some common symptoms, they also have distinct characteristics associated with health risks. Proper diagnosis and management are essential for addressing the specific needs of individuals affected by either condition.
PCOD or PCOS – which is more dangerous?
Polycystic Ovary Disorder (PCOD) and Polycystic Ovary Syndrome (PCOS) are two common hormonal disorders affecting women worldwide. While they share similarities, they also have distinct characteristics and implications for health. One question often arises: which of these conditions is more dangerous? Let’s delve into the intricacies of both PCOD and PCOS to understand their respective risks.
Unveiling PCOD and PCOS:
Polycystic Ovary Disorder (PCOD): PCOD is characterized by the presence of multiple cysts on the ovaries, hormonal imbalances, and menstrual irregularities. It primarily affects the ovaries and reproductive system, leading to symptoms such as irregular periods, ovarian cysts, and difficulties conceiving.
Polycystic Ovary Syndrome (PCOS): PCOS is a broader syndrome encompassing ovarian cysts, hormonal imbalances, and metabolic disturbances. In addition to reproductive issues, it often involves insulin resistance, obesity, hirsutism (excessive hair growth), acne, and increased risks of type 2 diabetes and cardiovascular disease.
Understanding the Risks:
PCOD: While PCOD primarily affects fertility and menstrual regularity, it can still impact overall health if left untreated. Prolonged menstrual irregularities may increase the risk of endometrial hyperplasia (thickening of the uterine lining) and potentially endometrial cancer. Furthermore, hormonal imbalances associated with PCOD can contribute to mood swings, depression, and anxiety, affecting mental well-being.
PCOS: PCOS is often considered more complex and potentially more dangerous due to its broader spectrum of symptoms and associated metabolic complications. Insulin resistance, a hallmark of PCOS, can lead to metabolic syndrome, type 2 diabetes, and cardiovascular disease. Moreover, irregular menstrual cycles in PCOS increase the risk of endometrial hyperplasia and cancer, posing significant health concerns.
Managing the Risks:
PCOD: Early diagnosis and proper management of PCOD are essential to mitigate potential risks. Lifestyle modifications such as regular exercise, a balanced diet, and weight management can help improve hormonal balance and menstrual regularity. In some cases, hormonal therapy may be prescribed to regulate menstrual cycles and reduce the risk of endometrial complications.
PCOS: Managing PCOS involves a multifaceted approach targeting hormonal regulation, metabolic health, and symptom management. Lifestyle interventions, including dietary changes and exercise, are crucial for managing insulin resistance and preventing metabolic complications. Medications such as oral contraceptives, anti-androgens, and insulin-sensitizing agents may be prescribed to address hormonal imbalances and symptoms. Fertility treatments may also be necessary for women with PCOS struggling to conceive.
While both PCOD and PCOS present significant health risks, PCOS is generally considered more dangerous due to its broader range of symptoms and associated metabolic disturbances. However, early diagnosis, lifestyle modifications, and appropriate medical interventions can help mitigate these risks and improve outcomes for individuals affected by either condition.
It is essential for individuals experiencing symptoms of PCOD or PCOS to seek medical attention for proper diagnosis and personalized treatment. With proactive management and support, women can effectively navigate these hormonal disorders and safeguard their health and well-being.



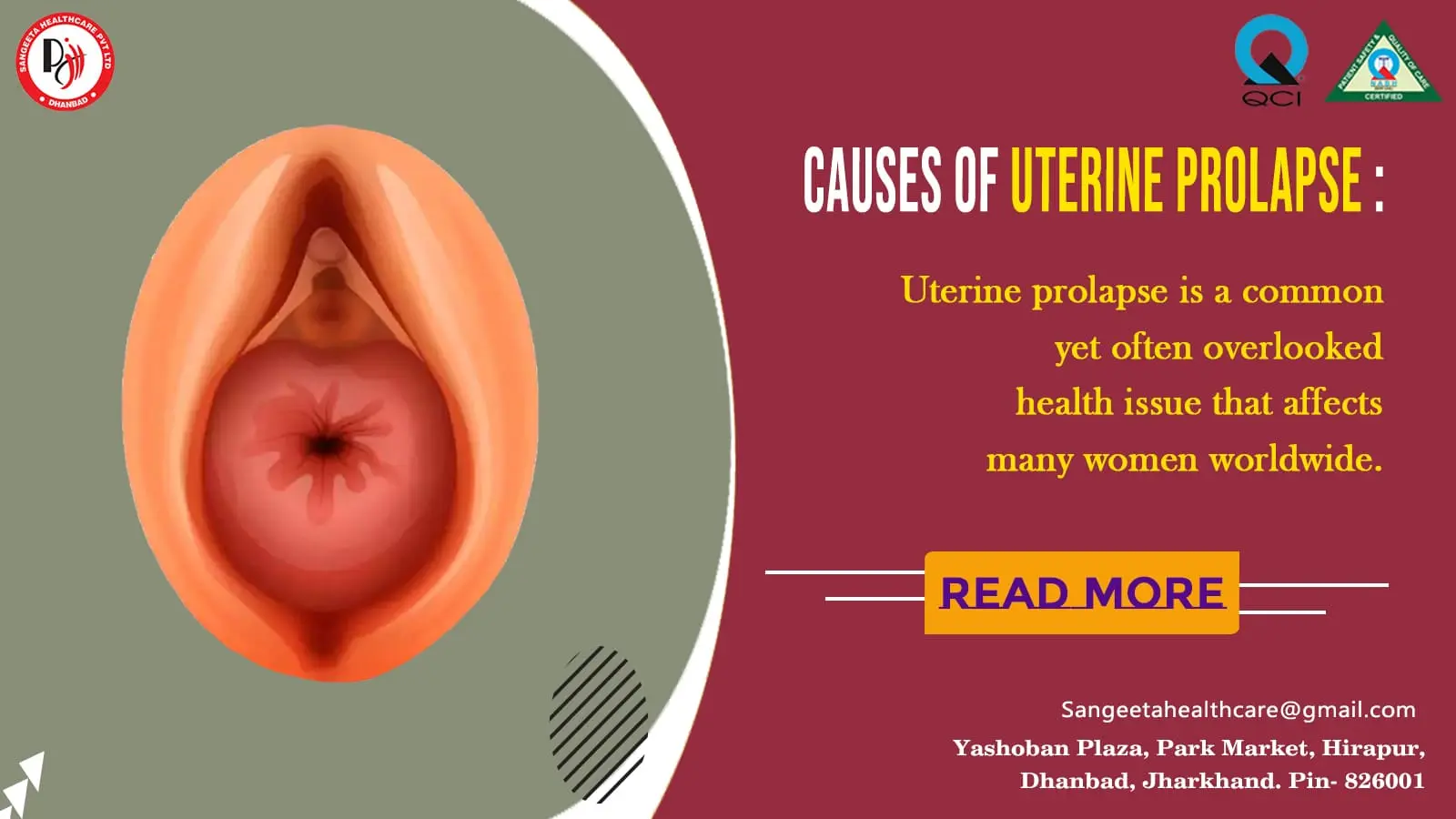
 Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.
Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.




















 Symptoms:
Symptoms:
