Endometrial Cancer

Endometrial cancer is a prevalent form of cancer that affects the lining of the uterus, known as the endometrium. While it primarily occurs in postmenopausal women, it can also affect younger women. Understanding the symptoms, causes, risk factors, and available treatment options is crucial for early detection and effective management of this condition.
Symptoms:
Endometrial cancer often presents with symptoms that may initially seem benign but should not be ignored. These symptoms include abnormal vaginal bleeding, such as bleeding between periods or after menopause, pelvic pain or pressure, and unusual vaginal discharge. It’s essential to consult a healthcare professional if experiencing any of these symptoms, as early detection can significantly improve treatment outcomes.
Causes and Risk Factors:
The exact cause of endometrial cancer is not fully understood, but several factors increase the risk of developing it. One primary risk factor is increased exposure to estrogen without the balancing influence of progesterone. This hormonal imbalance can occur due to various factors, including obesity, hormone therapy without progesterone, certain medications, and conditions such as polycystic ovary syndrome (PCOS). Other risk factors include advancing age, a history of endometrial hyperplasia, diabetes, and a family history of endometrial or colorectal cancer.
Diagnosis:
Diagnosing endometrial cancer typically involves a combination of medical history evaluation, pelvic exams, imaging tests (such as transvaginal ultrasound), and endometrial biopsy. Endometrial biopsy, where a sample of tissue is taken from the lining of the uterus for examination, is the most definitive diagnostic test.
Treatment Options: Treatment for endometrial cancer depends on several factors, including the stage and grade of the cancer, as well as the individual’s overall health and preferences. Common treatment options include:
- Surgery: Surgery is often the primary treatment for endometrial cancer and may involve a hysterectomy (removal of the uterus) with or without removal of nearby lymph nodes.
- Radiation Therapy: Radiation therapy uses high-energy beams to kill cancer cells and may be recommended after surgery to destroy any remaining cancer cells or as a primary treatment for those who cannot undergo surgery.
- Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells and may be used in combination with surgery or radiation therapy, especially for advanced or recurrent endometrial cancer.
- Hormone Therapy: Hormone therapy may be recommended for women with advanced endometrial cancer that has spread beyond the uterus and responds to hormones. This treatment aims to block the effects of estrogen on cancer cells.
Endometrial cancer is a serious condition that requires prompt medical attention. By understanding the symptoms, causes, and risk factors associated with this disease, individuals can take proactive steps to reduce their risk and seek early detection and treatment when necessary. With advancements in medical technology and treatment options, the prognosis for endometrial cancer continues to improve, offering hope to those affected by this disease. Regular screenings and maintaining a healthy lifestyle are essential in the prevention and early detection of endometrial cancer. If you experience any symptoms or have concerns about your health, don’t hesitate to consult a healthcare professional.
Can I get pregnant with endometrial cancer- Know the Answer
The diagnosis of endometrial cancer can be daunting, especially for women who have dreams of starting a family. One common question that arises is whether it’s possible to get pregnant with endometrial cancer. The answer to this question is not straightforward and depends on various factors, including the stage of cancer, treatment options, and individual circumstances. Let’s delve deeper into this complex topic to understand the possibilities and challenges associated with fertility and endometrial cancer.
-
Fertility Challenges:
Endometrial cancer affects the lining of the uterus, potentially impacting fertility. In advanced stages or cases where aggressive treatment is necessary, fertility preservation may not be feasible. Standard treatments for endometrial cancer often involve the removal of the uterus (hysterectomy) and other reproductive organs, making natural conception impossible after treatment.
-
Fertility-Sparing Options:
However, for women diagnosed with early-stage endometrial cancer who wish to preserve their fertility, there are fertility-sparing treatment options available. These treatments aim to remove or destroy cancerous tissue while preserving the uterus and fertility. Hormone therapy, such as progestin therapy, may be used to shrink or stabilize the tumor, allowing women to conceive after treatment. Additionally, minimally invasive surgical techniques, such as hysteroscopy resection or endometrial ablation, may be considered to remove cancerous lesions while preserving the uterus.
-
Individualized Approach:
The decision regarding fertility preservation and treatment options for endometrial cancer should be highly individualized and based on factors such as the patient’s age, cancer stage and grade, overall health, and fertility goals. It’s essential for women diagnosed with endometrial cancer to discuss their fertility preservation options with a multidisciplinary team of healthcare professionals, including gynecologic oncologists, reproductive endocrinologists, and fertility specialists. These experts can provide personalized guidance and explore various treatment pathways that prioritize both cancer management and fertility preservation.
-
Alternative Paths to Parenthood:
For women who are unable to conceive naturally after endometrial cancer treatment or fertility-sparing interventions, alternative paths to parenthood may be considered. Options such as adoption, surrogacy, or egg donation can provide fulfilling avenues for building a family.
-
Emotional Support:
Navigating the journey of fertility and endometrial cancer can evoke a range of emotions, including anxiety, grief, and uncertainty. It’s crucial for individuals facing this challenge to seek emotional support from loved ones, support groups, or mental health professionals. Open communication with healthcare providers and sharing concerns about fertility and family planning can also alleviate some of the emotional burden associated with the diagnosis and treatment of endometrial cancer.
While endometrial cancer poses challenges to fertility, it’s possible for some women to conceive with early diagnosis and appropriate treatment. Fertility-sparing options and advancements in reproductive medicine offer hope to those desiring to preserve their ability to have children. However, each case is unique, and decisions regarding fertility preservation and cancer treatment should be made in collaboration with healthcare providers, considering individual circumstances and preferences. Irrespective of the outcome, support and resources are available to help individuals navigate the complexities of fertility and endometrial cancer with resilience and hope.
How does endometrial cancer spread?
Endometrial cancer, a type of cancer that originates in the lining of the uterus, can be a frightening diagnosis. One of the most crucial aspects of managing endometrial cancer is understanding how it spreads, or metastasizes, throughout the body. By comprehending the mechanisms of metastasis, patients, caregivers, and healthcare professionals can make informed decisions about treatment and care strategies. Let’s delve into the intricate process of how endometrial cancer spreads and its implications for patients.
Understanding Metastasis:
Metastasis is the process by which cancer cells break away from the primary tumor and spread to other parts of the body, forming secondary tumors. In endometrial cancer, metastasis typically involves the spread of cancer cells from the uterus to nearby organs or tissues within the pelvis, such as the ovaries, fallopian tubes, cervix, or vagina. Additionally, endometrial cancer can metastasize to distant sites, including the lymph nodes, lungs, liver, and bones, through the bloodstream or lymphatic system.
Factors Influencing Metastasis:
Several factors influence the metastatic spread of endometrial cancer, including the cancer’s stage, grade, and subtype, as well as individual patient characteristics. Higher-grade tumors, for example, tend to be more aggressive and have a greater propensity for metastasis than lower-grade tumors. Similarly, advanced-stage endometrial cancer, where the disease has spread beyond the uterus, is more likely to metastasize to distant sites.
Routes of Spread:
Endometrial cancer can spread through various routes, including direct extension, lymphatic spread, and hematogenous (blood) spread. Direct extension occurs when cancer cells invade nearby tissues or organs, such as the cervix or vagina, through direct contact. Lymphatic spread involves the dissemination of cancer cells to regional lymph nodes, such as the pelvic and para-aortic lymph nodes, via the lymphatic vessels. Hematogenous spread occurs when cancer cells enter the bloodstream and travel to distant organs, such as the lungs, liver, or bones, where they can establish secondary tumors.
Clinical Implications:
The spread of endometrial cancer has significant clinical implications for patient prognosis and treatment planning. Metastatic disease often indicates a more advanced stage of cancer and may require more aggressive treatment approaches, such as surgery, radiation therapy, chemotherapy, targeted therapy, or hormone therapy, depending on the extent and location of metastasis. Additionally, metastatic endometrial cancer may necessitate ongoing monitoring and management to address disease progression and control symptoms.
Future Directions:
Advances in cancer research, including molecular profiling and targeted therapies, offer promising avenues for understanding and combating the metastatic spread of endometrial cancer. By elucidating the underlying molecular mechanisms driving metastasis, researchers aim to develop more effective treatments that specifically target metastatic lesions while minimizing systemic side effects.
Understanding how endometrial cancer spreads is essential for guiding treatment decisions and improving patient outcomes. By recognizing the factors influencing metastasis, healthcare professionals can tailor treatment approaches to individual patients and optimize disease management strategies. Moreover, ongoing research efforts aimed at unravelling the complexities of metastasis hold the potential to revolutionize the treatment landscape for endometrial cancer, offering hope for improved survival and quality of life for patients facing this life-threatening ailment.
What are the symptoms of endometrial cancer?
Endometrial cancer often presents with symptoms that may initially seem benign but should not be ignored. Early detection of these symptoms can lead to timely diagnosis and treatment, which is crucial for improving outcomes. Here are some of the common indications of endometrial cancer:
- Abnormal Vaginal Bleeding: The most common symptom of endometrial cancer is abnormal vaginal bleeding, which may include:
- Postmenopausal bleeding: Bleeding that occurs after menopause, which is defined as the absence of menstruation for 12 consecutive months.
- Irregular menstrual bleeding: Unusual bleeding between periods or changes in menstrual patterns, such as heavier or longer periods.
- Pelvic Pain or Pressure: Some women with endometrial cancer may experience pelvic pain or pressure, which can vary in intensity and may be persistent or intermittent.
- Unusual Vaginal Discharge: Endometrial cancer can cause changes in vaginal discharge, such as:
- Watery or blood-tinged discharge
- Discharge that may be foul-smelling or different from usual
- Painful Urination or Intercourse: In some cases, endometrial cancer may cause discomfort or pain during urination or sexual intercourse.
- Enlargement of the Uterus: Endometrial cancer may lead to the enlargement of the uterus, which can sometimes be felt as a mass or lump in the lower abdomen.
It’s important to note that while these symptoms can be indicative of endometrial cancer, they can also be caused by other gynecological conditions. However, any persistent or concerning symptoms should prompt a consultation with a healthcare provider for further evaluation and appropriate diagnostic testing, such as pelvic examination, ultrasound, or endometrial biopsy.
Early detection of endometrial cancer is associated with better treatment outcomes, so it’s essential not to ignore any signs or symptoms that may be suggestive of this condition. If you experience any of the symptoms mentioned above, don’t hesitate to seek medical attention promptly. Your healthcare provider can conduct the necessary tests to determine the cause of your symptoms and recommend appropriate treatment options.
Is uterine cancer and endometrial cancer the same thing?
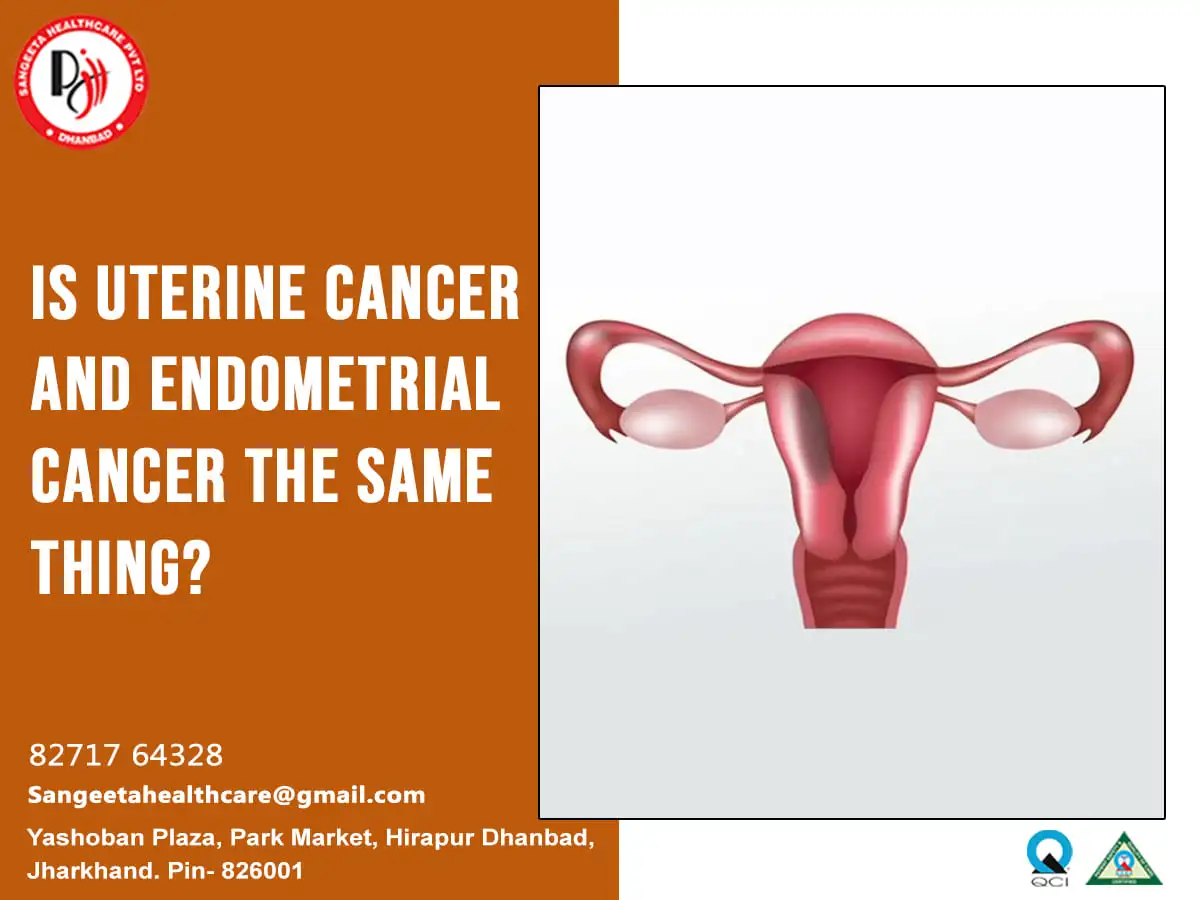
Uterine cancer and endometrial cancer are often used interchangeably, but they are not precisely the same thing. However, they are closely related, and the vast majority of uterine cancers are endometrial cancers. Let’s shed light on the distinction between them:
-
Endometrial Cancer:
- Endometrial cancer specifically refers to cancer that originates in the lining of the uterus, known as the endometrium. This type of cancer accounts for the majority (about 80-90%) of uterine cancers.
- Endometrial cancer typically develops in the innermost layer of the uterus, where the endometrium resides. It often presents with symptoms such as abnormal vaginal bleeding, pelvic pain, or unusual vaginal discharge.
- Risk factors for endometrial cancer include hormonal imbalances, obesity, diabetes, estrogen therapy without progesterone, and a family history of certain cancers.
-
Uterine Cancer:
- Uterine cancer is a broader term that encompasses cancers arising from various parts of the uterus, including the endometrium, myometrium (muscle layer), and other rare types of uterine tumors.
- While the majority of uterine cancers are endometrial cancers, a small percentage (about 10-20%) are uterine sarcomas, which develop from the muscle or other tissues of the uterus.
- Uterine sarcomas are less common than endometrial cancers and generally have different risk factors, clinical features, and treatment approaches.
In summary, while endometrial cancer specifically refers to cancer originating in the endometrium, uterine cancer is a broader term encompassing cancers arising from various parts of the uterus. However, in most cases, when people refer to uterine cancer, they are typically referring to endometrial cancer due to its higher prevalence. It’s essential to consult with healthcare professionals for accurate diagnosis, staging, and treatment planning for any suspected uterine or endometrial cancer.



 Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.
Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.