Empowering Women’s Health: Breaking the Silence on Ovarian Cysts
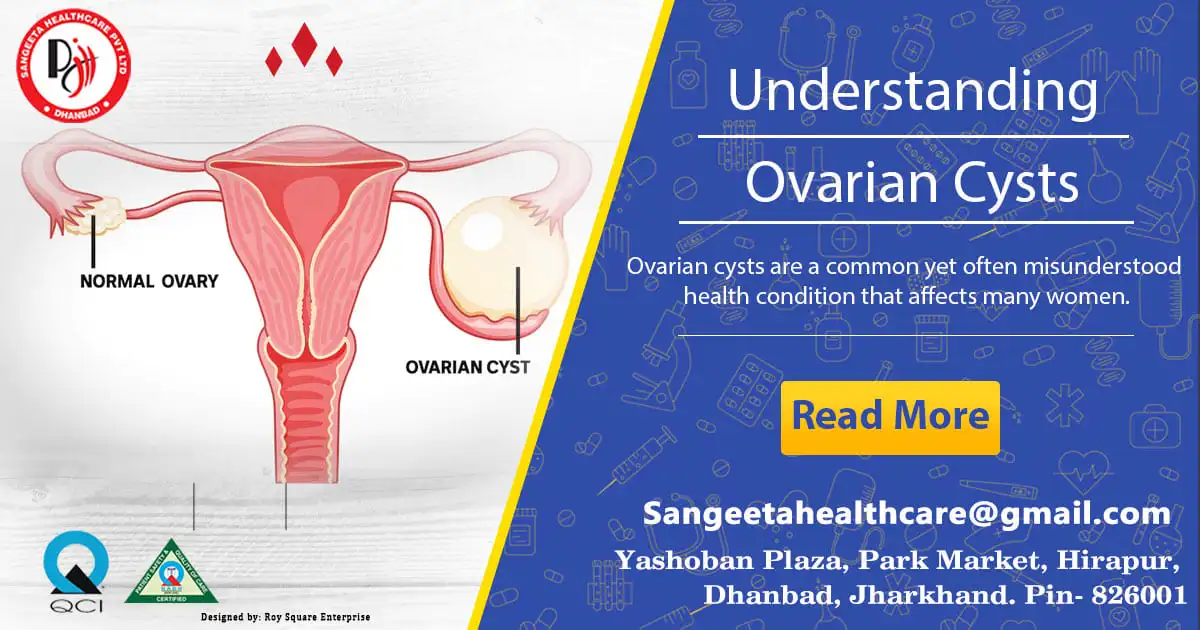
Ovarian Cysts
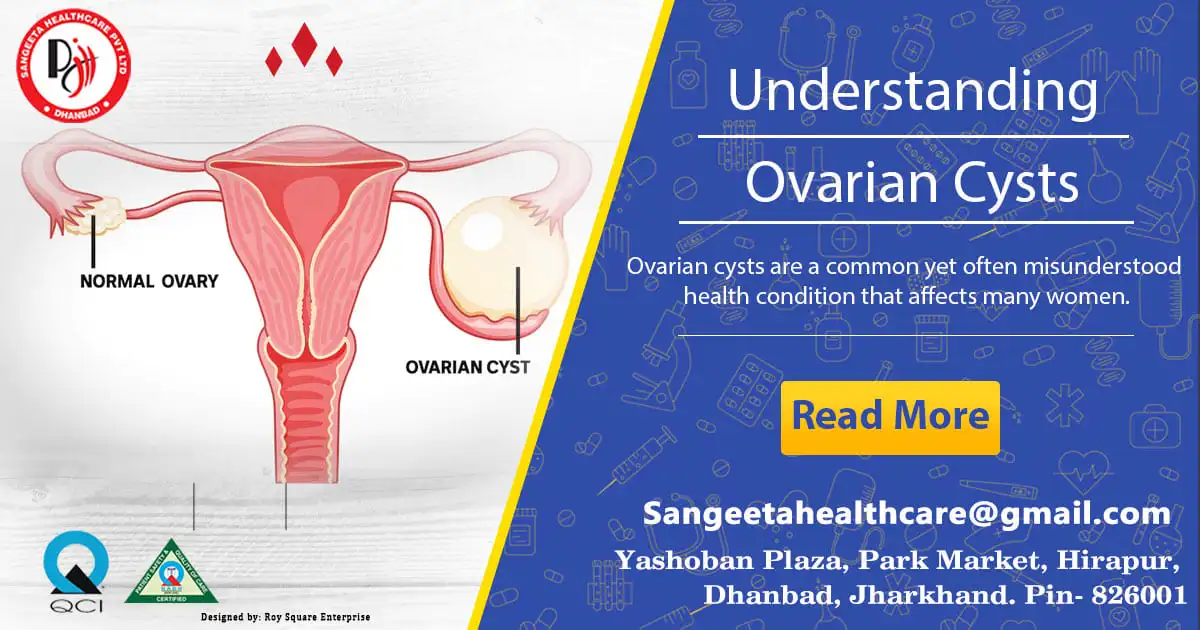
Ovarian cysts are a common yet often misunderstood health condition that affects many women. These fluid-filled sacs range in size from little to enormous and can form on or inside the ovaries. While most ovarian cysts are harmless and resolve on their own, some may cause discomfort or pose more serious health risks. In this blog, we will delve into the world of ovarian cysts, exploring their causes, symptoms, diagnosis, and treatment options.
Understanding Ovarian Cysts:
1. Types of Ovarian Cysts:
• Functional Cysts: The most typical ones, they frequently develop during the menstrual cycle. They consist of corpus luteum cysts and follicular cysts.
• Dermoid Cysts: These cysts contain tissues like hair, skin, or teeth and are present from birth.
• Endometriomas: Formed due to endometriosis, these cysts develop when endometrial tissue grows outside the uterus.
• Cystadenomas: These cysts develop on the surface of the ovary and are filled with a watery or mucous-like substance.
2. Causes of Ovarian Cysts:
• Hormonal imbalances during the menstrual cycle.
• Endometriosis.
• Pregnancy-related cysts.
• Polycystic Ovary Syndrome (PCOS).
• Pelvic infections.
Common Symptoms:
1. Pain:
• Dull aching in the lower abdomen.
• Pain in pelvic region during or prior to the menstrual cycle.
• Pain during intercourse.
2. Changes in Menstrual Cycle:
• Irregular periods.
• Heavier or lighter menstrual flow.
• Changes in the duration of the menstrual cycle.
3. Other Symptoms:
• Bloating.
• Difficulty emptying the bladder completely.
• Frequent urination.
Diagnosis and Medical Evaluation:
1. Pelvic Examination:
• Feeling for the presence, size, and shape of cysts.
2. Ultrasound:
• Imaging tests to visualize the cyst’s size, shape, and composition.
3. Blood Tests:
• To check for hormonal irregularities or tumor markers.
Treatment Options:
1. Watchful Waiting:
• Numerous cysts clear up on their own without medical assistance.
2. Medications:
• Hormonal birth control to regulate the menstrual cycle.
• Pain relievers for discomfort.
3. Surgery:
• Cystectomy, in which the cyst is removed but the ovary is left intact.
• Oophorectomy if the cyst is cancerous or the entire ovary needs removal.
Within the intricate world of reproductive anatomy, the bilocular ovary stands out as a unique and fascinating feature. This specialized type of ovary, characterized by its bilobed structure, plays a crucial role in the reproductive processes of certain organisms.
Understanding Bilocular Ovary:
1. Structure:
• A bilocular ovary is distinguished by its two distinct lobes or compartments.
• Each lobe functions as an independent unit, housing its set of ovarian follicles and ova.
2. Occurrence in Organisms:
• Bilocular ovaries are commonly found in various invertebrates, such as insects, crustaceans, and certain mollusks.
• This unique structure is an evolutionary adaptation that contributes to the reproductive strategies of these organisms.
3. Reproductive Significance:
• Improved Reproductive Efficiency: The bilocular structure allows for a more organized and efficient reproductive process. Each lobe can develop and release ova independently, increasing the overall reproductive output.
4. Oogenesis in Bilocular Ovary:
• Oogenesis, the process of egg cell development, occurs separately in each lobe.
• This independence enables the organism to produce a larger number of eggs simultaneously, enhancing the chances of successful fertilization.
5. Adaptations for Environmental Challenges:
• The bilocular ovary structure can be an adaptive response to specific environmental conditions. Organisms with bilocular ovaries may have evolved this feature to cope with challenges such as predation, fluctuating temperatures, or limited resources.
6. Examples in Nature:
• Bees and wasps are examples of insects that possess bilocular ovaries. The bilobed structure contributes to their intricate social structures and reproductive strategies.
The bilocular ovary, with its distinctive structure and specialized functions, exemplifies the incredible diversity of reproductive adaptations in the natural world. As we uncover the mysteries of bilocular ovaries, we gain valuable insights into the evolutionary strategies that different species have developed to ensure the continuation of their genetic legacy. Whether in the buzzing world of insects or the depths of the ocean with crustaceans, the bilocular ovary serves as a testament to the marvels of nature’s ingenuity in the pursuit of reproductive success.
The human body is a marvel of complexity, and within the intricate landscape of pelvic anatomy, cystic lesions can emerge as enigmatic entities. These fluid-filled sacs, often referred to as “cyests,” can be found in various regions of the pelvis, raising questions about their origins, symptoms, and potential implications for health. Now, in this blog, we will embark on a journey to unravel the mysteries of cystic lesions in the pelvis, shedding light on their characteristics, diagnostic processes, and the importance of proactive healthcare.

Understanding Cystic Lesions:
1. Definition of Cystic Lesions:
• Cystic lesions are fluid-filled sacs that can develop in different structures within the pelvic region, including the ovaries, fallopian tubes, or other surrounding tissues.
2. Types of Pelvic Cysts:
• Ovarian Cysts: Fluid-filled sacs that form on or within the ovaries, often associated with the female reproductive system.
• Paraovarian Cysts: Cysts located near the ovaries, arising from the vestiges of embryonic structures.
• Endometriomas: Cysts resulting from the presence of endometrial tissue outside the uterus, commonly found in the pelvic cavity.
Common Symptoms:
1. Pelvic Pain:
• Dull or sharp pain in the lower abdomen, varying in intensity.
2. Changes in Menstrual Cycle:
• Irregular periods.
• Heavy or painful menstrual flow.
3. Discomfort during Intercourse:
• Pain or discomfort during sexual activity.
4. Urinary or Bowel Issues:
• Having trouble entirely emptying the bladder or urinating often.
• Changes in bowel habits.
Diagnostic Approaches:
1. Imaging Tests:
• Ultrasound: Visualizing the cyst’s size, shape, and composition.
• MRI or CT scans: Providing detailed cross-sectional images for further analysis.
2. Blood Tests:
• CA-125 test: Assessing the presence of specific proteins associated with ovarian cysts.
3. Biopsy:
• In some cases, a biopsy may be performed to analyze the tissue composition of the cyst.
Management and Treatment:
1. Watchful Waiting:
• Many cysts heal without the need for medical assistance.
2. Medications:
• Pain relievers for discomfort.
• Intake of hormonal contraceptives for menstrual cycle regulation.
3. Surgery:
• Cystectomy: Surgical removal of the cyst while preserving the surrounding tissues.
• Hysterectomy: In more severe cases, removal of the uterus and possibly other reproductive organs.
Cystic lesions in the pelvis are a complex and diverse group of conditions, and their impact on an individual’s health can vary. Timely diagnosis and appropriate management are crucial for addressing any potential complications and ensuring the well-being of those affected. By understanding the intricacies of these cystic entities, individuals and healthcare professionals alike can work together to navigate the path toward optimal pelvic health.
The presence of mild fluid in the pod typically refers to a small amount of fluid accumulation in the Pouch of Douglas, a space between the rectum and the back wall of the uterus in women. While mild fluid in the pod is a common finding and may not necessarily indicate a serious issue, it’s important to be aware of potential symptoms or contributing factors. Here are some aspects to consider:
Common Symptoms:
1. Pelvic Discomfort or Pain:
• Mild fluid in the pod may sometimes be associated with pelvic discomfort or a dull ache.
2. Menstrual Irregularities:
• Some individuals may experience changes in their menstrual cycle or abnormal bleeding.
3. Pain during Intercourse:
• Sexual activity may cause discomfort or pain in individuals with fluid in the pod.
4. Urinary Symptoms:
• Frequent urination or changes in bladder habits may occur.
5. Gastrointestinal Issues:
• Constipation or changes in bowel habits could be associated with mild fluid in the pod.
Possible Causes:
1. Normal Physiological Variation:
• In some cases, the presence of mild fluid in the pod may be a normal physiological variation without any underlying pathology.
2. Menstrual Cycle-related Changes:
• Hormonal fluctuations during the menstrual cycle can influence the amount of fluid in the Pouch of Douglas.
3. Pelvic Infections or Inflammation:
• Infections or inflammatory conditions in the pelvic region may lead to fluid accumulation.
4. Endometriosis:
• Endometriosis, a condition where endometrial tissue grows outside the uterus, can contribute to fluid accumulation in the pelvic cavity.
When to Seek Medical Attention:
While mild fluid in the pod is often benign, it’s important to consult with a healthcare professional if you experience:
• Persistent or worsening pelvic pain.
• Unexplained changes in menstrual patterns.
• Pain during sexual intercourse.
• Any other concerning symptoms.
Diagnostic Procedures:
1. Pelvic Ultrasound:
• An ultrasound may be performed to visualize the pelvic organs and assess the amount of fluid in the pod.
2. Physical Examination:
• A gynecological examination can help in evaluating the presence of any abnormalities.
3. Blood Tests:
• In cases where infection is suspected, blood tests may be conducted to check for elevated inflammatory markers.
4. Further Imaging Studies:
• Depending on the clinical presentation, additional imaging studies such as MRI or CT scans may be recommended.
Treatment:
Treatment depends on the underlying cause. In many cases, mild fluid in the pod may not require specific intervention. However, if an underlying condition is identified, targeted treatment may be recommended.
It’s crucial to communicate openly with your healthcare provider, provide a detailed medical history, and undergo any necessary diagnostic tests to determine the cause of the mild fluid in the pod and address any associated symptoms.
Understanding ovarian cysts is crucial for women’s health, as early detection and proper management can significantly impact outcomes. If you suspect you have an ovarian cyst or are experiencing symptoms, seeking prompt medical attention is essential. Remember, knowledge and awareness are powerful tools in managing and maintaining women’s reproductive health.


