Hormones are the body’s chemical messengers, playing a crucial role in regulating nearly every physiological process. Hormones play a vital role in keeping the body balanced by regulating metabolism, growth, mood, and reproductive health. But what happens when these hormones go out of sync? In this blog post, we’ll explore what hormones are, discuss common hormonal disorders, and uncover what causes hormonal imbalances. Whether you’re a medical professional or someone curious about your health, this guide will provide valuable insights into the fascinating world of hormones.
What Are Hormones?
Hormones are specialized chemicals produced by the endocrine glands, such as the thyroid, adrenal glands, pancreas, and pituitary gland. These glands release hormones directly into the bloodstream, where they travel to target organs and tissues to regulate their function. Think of hormones as the body’s internal communication system—they ensure that everything runs smoothly and efficiently.
Some of the most well-known hormones include:
– Insulin: Regulates blood sugar levels.
– Thyroid Hormones (T3 and T4): Control metabolism and energy production.
– Estrogen and Testosterone: Govern reproductive health and secondary sexual characteristics.
– Cortisol: Manages stress response and metabolism.
– Growth Hormone: It promotes tissue growth and repair.
Each hormone has a specific role, but they often work together in complex ways to maintain homeostasis (balance) in the body.
Common Hormonal Disorders
When hormones are not balanced, it can cause many health problems. Here are some of the most frequent hormonal disorders:
-
Hypothyroidism and Hyperthyroidism
The thyroid gland produces hormones that regulate metabolism. **Hypothyroidism** occurs when the thyroid is underactive, leading to symptoms like fatigue, weight gain, and depression. On the other hand, **hyperthyroidism** results from an overactive thyroid, causing weight loss, anxiety, and rapid heartbeat.
-
Diabetes
Diabetes is a condition where the body either doesn’t produce enough insulin (Type 1 Diabetes) or becomes resistant to insulin (Type 2 Diabetes). This leads to elevated blood sugar levels, which can damage organs over time.
-
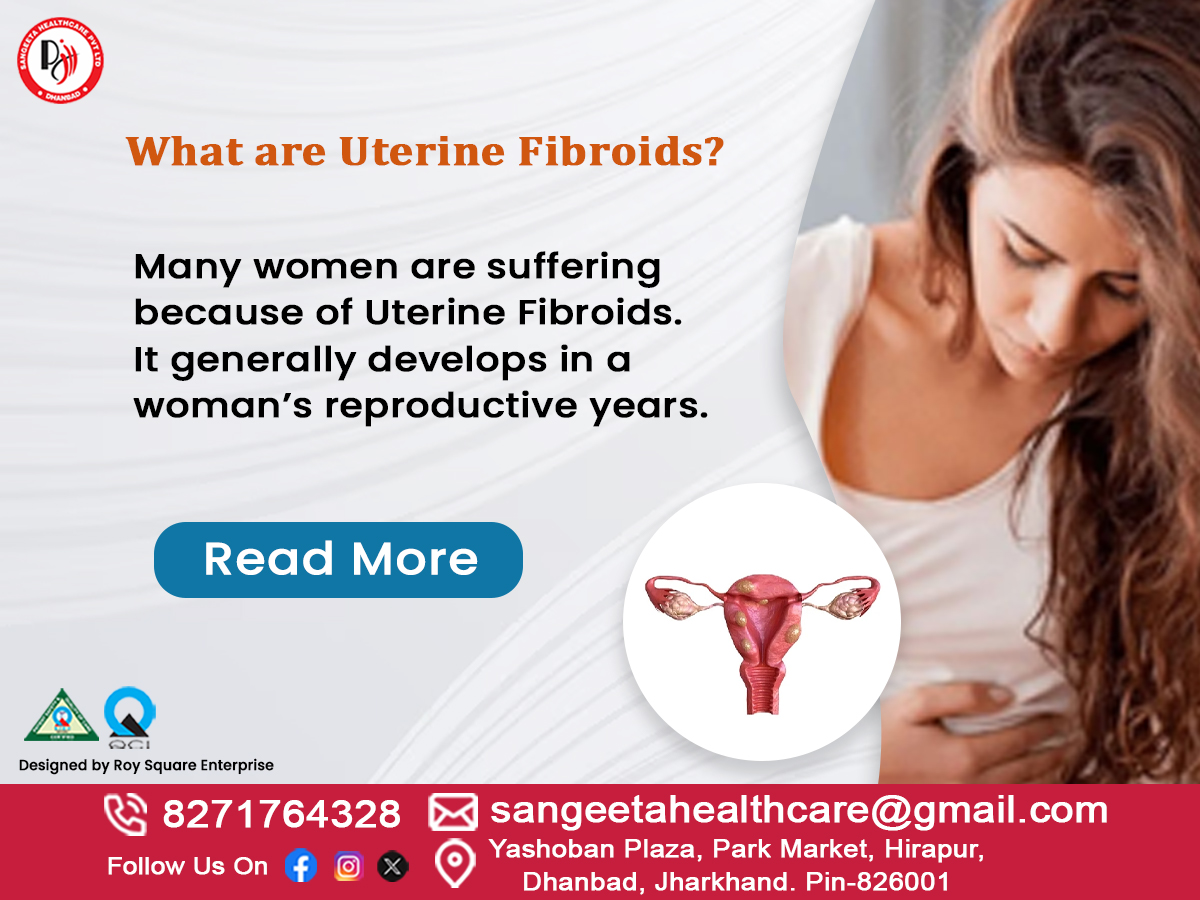
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a frequent hormonal condition affecting women during their childbearing years. It is characterized by irregular menstrual cycles, excess androgen levels, and ovarian cysts. Symptoms include weight gain, acne, and infertility.
-
Adrenal Insufficiency
The adrenal glands release cortisol, a hormone that assists the body in managing stress. Adrenal insufficiency, such as in Addison’s disease, occurs when the adrenal glands don’t produce enough cortisol, leading to fatigue, muscle weakness, and low blood pressure.
-
Growth Hormone Disorders
Too much or too little growth hormone can lead to disorders like **gigantism** (excessive growth) or **dwarfism** (stunted growth). In adults, growth hormone imbalances can cause muscle weakness, increased fat, and reduced bone density.
-
Menopause and Andropause
Menopause is a natural decline in estrogen levels in women, typically occurring in their late 40s or early 50s. Symptoms include hot flashes, mood swings, and bone density loss. Similarly, men experience a gradual decline in testosterone levels, known as **andropause**, which can lead to fatigue, reduced libido, and muscle loss.
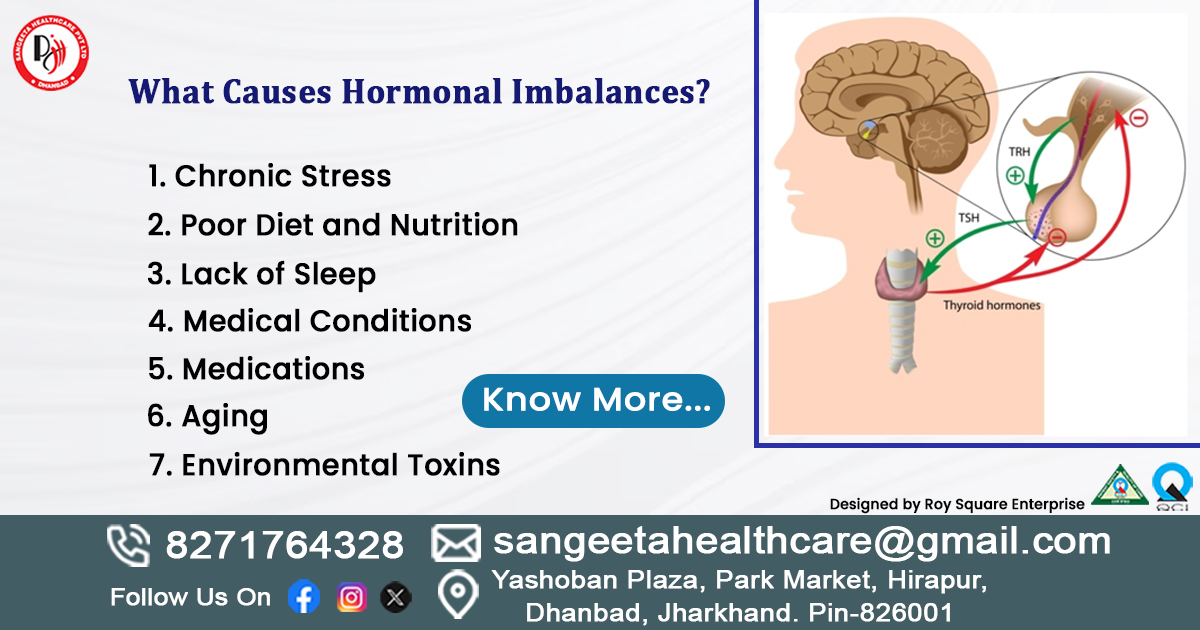
What Causes Hormonal Imbalances?
Hormonal imbalances can occur for a variety of reasons, ranging from lifestyle factors to underlying medical conditions. Here are some common causes:
-
Chronic Stress
Stress triggers the release of cortisol, the “stress hormone.” Prolonged stress can lead to elevated cortisol levels, disrupting the balance of other hormones like insulin and thyroid hormones.
-
Poor Diet and Nutrition
A diet high in processed foods, sugar, and unhealthy fats can interfere with hormone production and regulation. For example, excessive sugar intake can lead to insulin resistance, a precursor to Type 2 Diabetes.
-
Lack of Sleep
Sleep is essential for hormone regulation. Disrupted sleep patterns can affect the production of growth hormone, cortisol, and even reproductive hormones.
-
Medical Conditions
Certain medical conditions, such as tumors on endocrine glands, autoimmune diseases, or genetic disorders, can disrupt hormone production. For instance, Hashimoto’s thyroiditis is an autoimmune condition that damages the thyroid gland, leading to hypothyroidism.
-
Medications
Some medications, including steroids, birth control pills, and hormone replacement therapies, can alter hormone levels. Always consult your healthcare provider about potential side effects.
-
Aging
As we age, the production of certain hormones naturally declines. For example, women experience a drop in estrogen during menopause, while men see a gradual decrease in testosterone levels.
-
Environmental Toxins
Exposure to endocrine-disrupting chemicals (EDCs) found in plastics, pesticides, and personal care products can interfere with hormone function. These chemicals mimic or block natural hormones, leading to imbalances.
How to Maintain Hormonal Balance
Keeping your hormones balanced is essential for good health and a sense of well-being. Here are some practical tips:

- Eat a Balanced Diet: Focus on whole foods, lean proteins, healthy fats, and fiber. Avoid excessive sugar and processed foods.
- Exercise Regularly: Physical activity helps regulate insulin, cortisol, and other hormones.
- Manage Stress: Practice mindfulness, meditation, or yoga to keep stress levels in check.
- Get Enough Sleep: Make sure to get 7 to 9 hours of good, restful sleep every night.
- Avoid Toxins: Limit exposure to endocrine-disrupting chemicals by choosing natural products and reducing plastic use.
- Regular Check-Ups: Visit your healthcare provider for routine screenings and blood tests to monitor hormone levels.
When to Seek Medical Help
If you’re experiencing symptoms like unexplained weight changes, fatigue, mood swings, or irregular menstrual cycles, it’s important to consult a healthcare professional. Hormonal imbalances can often be diagnosed through blood tests and treated with lifestyle changes, medications, or hormone therapy.
Conclusion
Hormones are the unsung heroes of our bodies, quietly working behind the scenes to keep everything in balance. Understanding what hormones are, recognizing common hormonal disorders, and knowing what causes hormonal imbalances can empower you to take control of your health. Whether you’re a medical professional or someone curious about your well-being, staying informed is the first step toward achieving hormonal harmony.
If you suspect a hormonal imbalance, don’t hesitate to reach out to a healthcare provider. Early diagnosis and treatment can make a world of difference in your quality of life.
Few Myths About Hormones :
- Myth: Only Women Have Hormonal Issues
Truth: Men get hormonal imbalances too, like low testosterone or thyroid problems.
- Myth: Hormonal Imbalances Are Always Caused by Aging
Truth: Stress, diet, sleep, and toxins can disrupt hormones at any age.
- Myth: Eating Healthy Fixes All Hormonal Problems
Truth: Diet helps, but conditions like PCOS or diabetes need medical treatment.
- Myth: Birth Control Pills Fix Hormonal Imbalances
Truth: Birth control manages symptoms but doesn’t cure the root cause.
- Myth: Hormonal Imbalances Are Easy to Diagnose
Truth: Symptoms like fatigue or weight gain are vague—blood tests are often needed.
Here are some FAQs :
- What Are Hormones?
Answer: Hormones are chemical messengers that regulate processes like metabolism, growth, and mood.
- What Causes Hormonal Imbalances?
Answer: Stress, poor diet, lack of sleep, aging, medications, and medical conditions can disrupt hormones.
- Can Men Have Hormonal Imbalances?
Answer: Yes! Men can experience low testosterone, thyroid issues, or adrenal problems.
- What Are Common Symptoms of Hormonal Imbalances?
Answer: Fatigue, weight changes, mood swings, acne, irregular periods, and low libido are common signs.
- Can Hormonal Imbalances Be Cured?
Answer: Many can be managed with lifestyle changes, medications, or hormone therapy, but some require ongoing treatment.
- How Are Hormonal Imbalances Diagnosed?
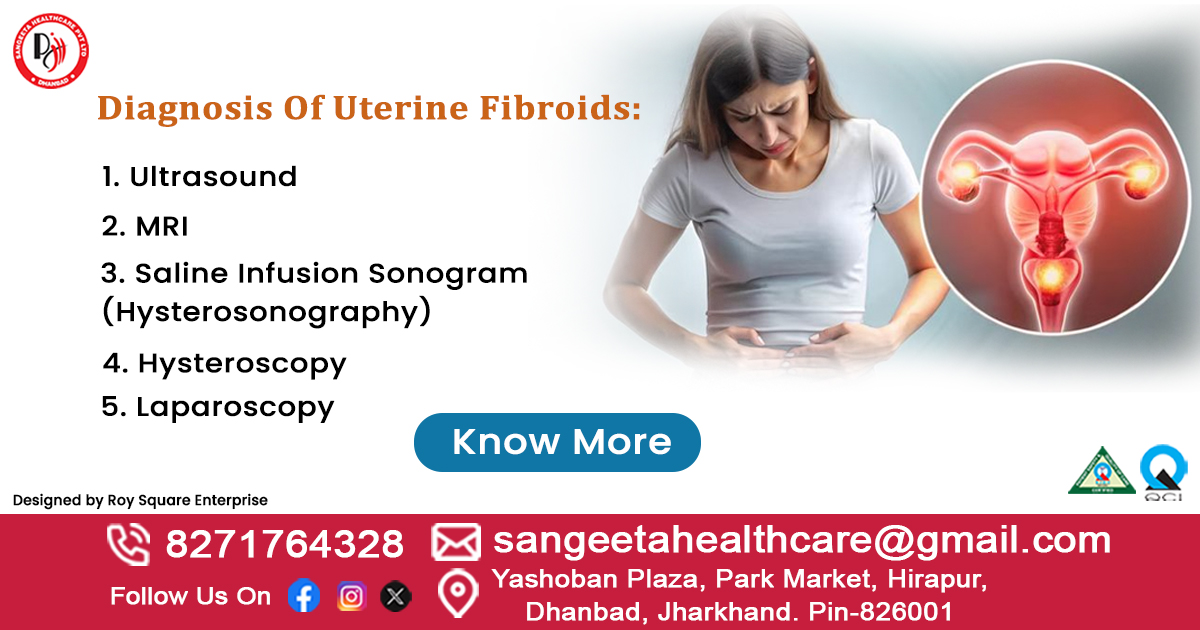
Answer: Blood tests, symptom evaluation, and sometimes imaging (like ultrasounds) help diagnose hormonal issues.
- Can Stress Affect Hormones?
Answer: Yes! Chronic stress raises cortisol levels, which can disrupt other hormones like insulin and thyroid hormones.
- Are Hormonal Imbalances Linked to Weight Gain?
Answer: Yes. Conditions like hypothyroidism, PCOS, and insulin resistance can make it harder to lose weight.