Your kidneys are the unsung heroes of your body—working silently around the clock to filter waste, balance fluids, and maintain your overall health. But what happens when these vital organs come under attack? A kidney infection, or pyelonephritis, is more than just a severe urinary tract infection (UTI). It’s a serious condition where harmful bacteria or pathogens invade the kidneys, turning a minor issue into a potentially life-threatening problem if left untreated.
Unlike a typical UTI, which may cause discomfort but often resolves with treatment, pyelonephritis can escalate quickly. Symptoms may start subtly—perhaps a dull backache, fever, or fatigue—but can rapidly progress to high fever, chills, nausea, and even sepsis if the infection spreads. The stakes are high: untreated kidney infections can lead to scarring, impaired kidney function, or even systemic infection, making early recognition and intervention crucial.
when it comes to kidney infections, knowledge isn’t just power—it’s prevention, timely care, and long-term well-being. Whether you’re a doctor, a nurse, or someone who’s never given their kidneys much thought, understanding pyelonephritis could make all the difference.
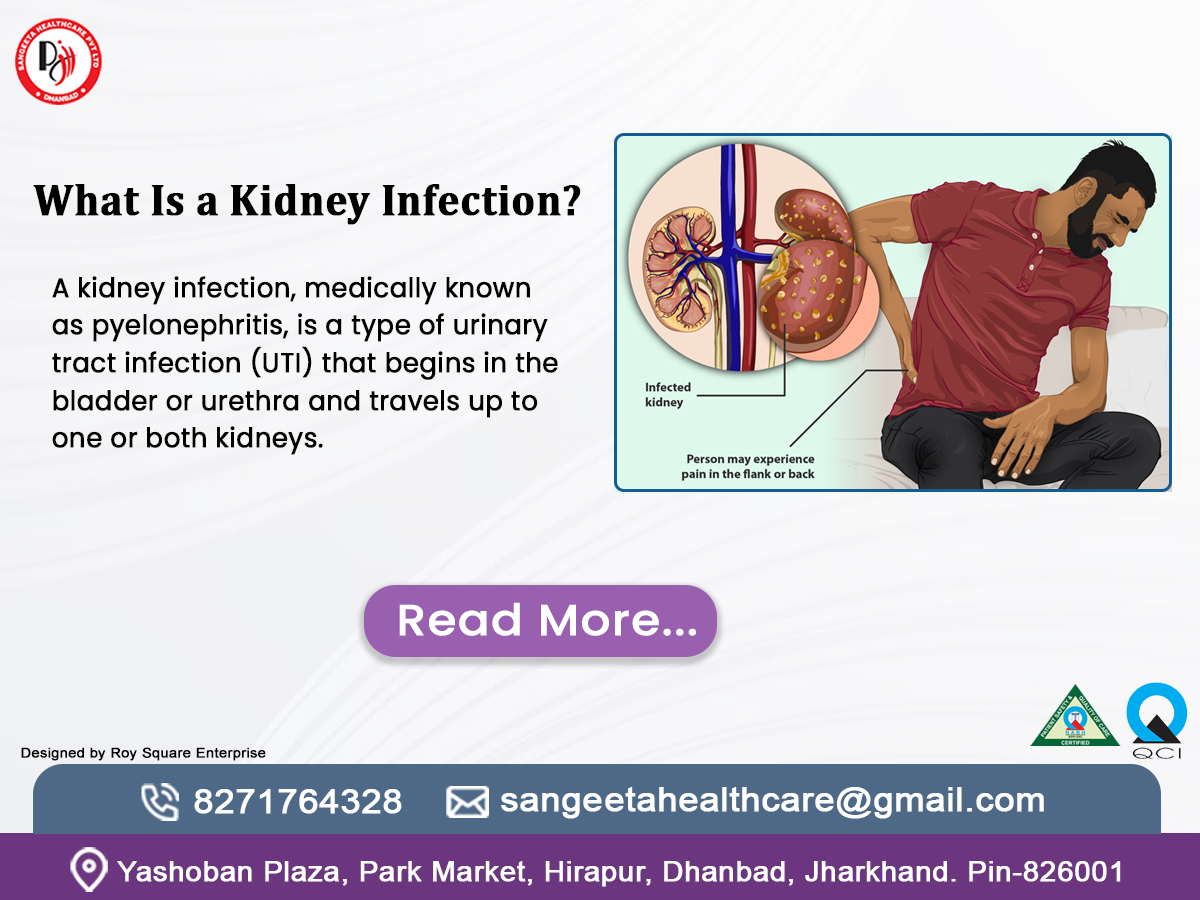
What Is a Kidney Infection?
A kidney infections, medically known as pyelonephritis, is a type of urinary tract infection (UTI) that begins in the bladder or urethra and travels up to one or both kidneys. The kidneys are vital organs responsible for filtering waste from your blood and producing urine. When bacteria or, rarely, fungi invade these organs, an infection can set in, leading to inflammation and potential complications.
Unlike a simple bladder infection, a kidney infection is more severe and requires prompt attention. It’s not just about discomfort—it can impair kidney function and, in extreme cases, lead to life-threatening conditions like sepsis. Understanding *what is a kidney infection* is the first step to recognizing its seriousness and taking action.
Causes of Kidney Infection

So, what sparks this troublesome condition? The causes of kidney infection are often tied to bacteria, with Escherichia coli (E. coli) being the most common culprit. This bacteria typically lives in the intestines but can migrate to the urinary tract, especially if hygiene practices falter or other risk factors come into play. Let’s take a closer look at the main reasons behind it.
Bacteria on the Move: The top troublemaker is Escherichia coli (E. coli), a bacteria that usually hangs out in your intestines. When it escapes its home turf—say, due to poor wiping habits (back to front, anyone?)—it sneaks into your urethra, climbs to your bladder, and storms your kidneys. It’s like an uninvited guest crashing your party and refusing to leave!
Blocked Pathways: Imagine your urinary system as a highway. Kidney stones, an enlarged prostate, or even a quirky birth defect can jam traffic, slowing urine flow. This backup creates a cozy swamp for bacteria to multiply, setting the stage for infection. It’s less of a road trip and more of a roadblock disaster.
Bladder Trouble Escalating: Most kidney infections start as a lower urinary tract infection (UTI) that’s ignored or undertreated. That pesky bladder bug doesn’t stay put—it hitches a ride upstream to your kidneys. Think of it as a small spark turning into a wildfire if you don’t douse it early.
Immune System Slump: If your body’s defenses are down—thanks to diabetes, HIV, or chemo—bacteria get a free pass to wreak havoc. Your kidneys become an easy target when your immune bouncers are off duty, letting infections slip through the cracks.
Catheter Culprits: Medical gear like urinary catheters can roll out the red carpet for bacteria. These tubes, used after surgery or for bladder issues, sometimes ferry germs straight into your system. It’s a helpful tool turned accidental traitor!
Gender Geography: Women, listen up—your shorter urethra (just 1.5 inches versus 8 in men) is like a shortcut for bacteria. Add in its proximity to the anus, and it’s no wonder women face this foe more often. Biology’s playing a sneaky game here.
Backflow Blues (Vesicoureteral Reflux): Normally, urine flows one way: down and out. But in some folks—especially kids—urine rebelliously flows back from the bladder to the kidneys. This reverse commute carries bacteria along for the ride, inviting infection to settle in.
For medical professionals, it’s worth noting that elderly patients might present atypical symptoms, such as confusion or delirium, rather than classic signs. Children, too, may show irritability or poor feeding. Identifying the signs of kidney infections early is essential for quick treatment.
Diagnosis of Kidney Infection
If you suspect a kidney infection, how is it confirmed? The “diagnosis of kidney infection” involves a mix of clinical evaluation and diagnostic tests. Here’s how healthcare providers typically approach it:
Chat and Check: First, your doctor plays interviewer, asking about your symptoms—fever, back pain, weird pee vibes?—and your health history (past UTIs? Kidney stones?). Then, they’ll press on your lower back to see if your kidneys flinch. It’s a hands-on start to the investigation!
Urine Sleuthing (Urinalysis): Next up, you pee in a cup—not glamorous, but crucial. This sample gets tested for bacteria, white blood cells (your body’s infection fighters), or blood. If the results light up like a crime scene, it’s a big hint your kidneys are in trouble.
Culture Club: To nab the exact villain, a urine culture grows the bacteria in a lab. It’s like putting out a “Wanted” poster—it tells your doc which germ’s causing chaos and which antibiotics will take it down. This step’s a game-changer for precision treatment.
Blood Work Backup: Sometimes, blood tests join the party. A high white blood cell count screams “infection!” while kidney function markers (like creatinine) show if the damage is spreading. It’s like checking the scoreboard to see how your kidneys are holding up.
Picture Perfect (Imaging): For tricky cases—think recurring infections or suspected blockages—doctors call in the big guns: a CT scan, ultrasound, or X-ray. These snapshots reveal stones, abscesses, or odd kidney shapes, painting a crystal-clear picture of what’s going on inside.
For medicos, imaging is particularly useful in recurrent cases or when “complications of kidney infection” like abscesses are suspected. The “diagnosis of kidney infection” bridges the gap between symptoms and effective treatment, ensuring nothing is overlooked.
Treatment for Kidney Infection
Once diagnosed, what’s next? The “treatment for kidney infection” focuses on eliminating the infection and relieving symptoms. Here’s how it’s typically managed: 
Antibiotic Arsenal: These meds are the heavy hitters. Your doctor picks one—like ciprofloxacin or amoxicillin—based on that urine culture, and you’ll take it for 7-14 days. It’s like sending in a SWAT team to clear out the bacterial squatters. Finish the whole course, or they might stage a comeback!
Hospital Heroics: If you’re super sick—high fever, puking, or pregnant—you might land in the hospital. IV antibiotics and fluids speed up the fight, hydrating you while zapping the infection. It’s intense care for when the stakes are sky-high.
Pain Tamers: That achy back or burning pee? Over-the-counter pals like ibuprofen or acetaminophen can dial down the misery. Think of them as your trusty sidekicks, keeping you comfy while the antibiotics do the heavy lifting. (Check with your doc first, though!)
Hydration Station: Chugging water isn’t just refreshing—it’s tactical. It flushes bacteria out of your system, like a power wash for your urinary tract. Aim for 8-10 glasses a day to keep the flow going and give those germs the boot.
Fixing the Source: Got a blockage like a kidney stone or a wonky prostate? Surgery might step in to clear the path. It’s like unclogging a drain—once the obstacle is gone, the infection’s got nowhere to hide.
Special Cases, Special Care: Pregnant? Kid-friendly antibiotics like nitrofurantoin keep the baby safe. Got recurring infections? A low-dose antibiotic shield might prevent round two. It’s a tailored treatment that fits your unique story.
Patients often wonder, “How is a kidney infection treated” beyond medication Staying hydrated is essential—drinking lots of water aids in washing away bacteria. Rest also supports recovery. For healthcare providers, tailoring antibiotics to local resistance patterns is critical, especially with rising antimicrobial resistance.
How Is a Kidney Infection Treated in Special Cases?
Diving deeper into “how is a kidney infection treated”, let’s consider special scenarios:
– Pregnant Women: Safe antibiotics like nitrofurantoin are chosen to protect the fetus, often with close monitoring.
– Children: Dosages are adjusted for age and weight, and reflux issues may need investigation.
– Recurrent Infections: Long-term, low-dose antibiotics or preventive strategies might be employed.
Treatment isn’t one-size-fits-all—it’s personalized to your health profile, making it both effective and safe.
Complications of Kidney Infection
Ignoring a kidney infection isn’t an option. Untreated or poorly managed infections can lead to “complications of kidney infection”, such as:
– Sepsis: A life-threatening infection spread to the bloodstream.
– Kidney Abscess: Pockets of pus that may require drainage.
– Chronic Kidney Disease: Repeated infections can scar the kidneys, impairing function.
– Pregnancy Risks: In expectant mothers, it can trigger preterm labor.
These risks underscore the importance of swift action. For medicos, monitoring for sepsis signs—like rapid heart rate or low blood pressure—is a priority in severe cases.
Kidney Infection Prevention
Can you stop a kidney infection before it starts? Absolutely! *Kidney infection prevention* hinges on simple yet effective habits:
– Stay Hydrated: Drink 6-8 glasses of water daily to flush your urinary system.
– Practice Good Hygiene: Wipe front to back, urinate after intercourse, and avoid holding urine for too long.
– Manage Chronic Conditions: Keep diabetes or kidney stones in check with regular care.
– Avoid Irritants: Cut back on excessive caffeine or alcohol, which can irritate the bladder.
Prevention is empowering—it puts you in control of your kidney health.
Home Remedies for Kidney Infection
Alongside medical treatment, *home remedies for kidney infection* can offer relief and support recovery:
– Cranberry Juice: Unsweetened cranberry juice may prevent bacteria from sticking to the urinary tract.
– Heat Therapy: A heating pad on your back can soothe flank pain.
– Herbal Teas: Parsley or dandelion tea might promote urination, but consult your doctor first.
– Probiotics: These can restore healthy gut and urinary bacteria balance.
While these remedies aren’t a cure, they complement professional care, especially for mild symptoms.
Why Kidney Infections Matter to Everyone
Kidney infections don’t discriminate—they can affect anyone, from kids to seniors, medicos to laypeople. For the general public, they’re a reminder to listen to your body. For healthcare professionals, they’re a call to educate patients and refine treatment protocols. By understanding “what is a kidney infection”, its causes, symptoms, diagnosis, and treatment, you’re better equipped to tackle it head-on.
Call to Action
Don’t let a kidney infection catch you off guard. If you’re experiencing symptoms like fever, back pain, or urinary changes, reach out to your healthcare provider today—early action can make all the difference. Want to stay ahead of the curve? Share this guide with friends, bookmark it for reference, or explore more health tips on our site. Your kidneys deserve the best—take charge of your wellness now!
Here are some FAQs :
- What exactly happens during a kidney infection?
A kidney infection, or pyelonephritis, is like an unwelcome guest crashing the party in your kidneys. It starts when bacteria—usually E. coli from your gut—sneak into your urinary tract and climb up to these vital organs. Once there, they set off inflammation, turning your kidneys into a battleground. This can disrupt their job of filtering blood and producing urine, leading to pain, fever, and more. Think of it as your body sounding an alarm that something’s gone rogue in your plumbing system!
- Can a kidney infection get healed on its own?
Here’s the straight talk: probably not. While a mild bladder infection might sometimes fade with extra water and rest, a kidney infection is a tougher beast. It’s deeper, more serious, and usually needs antibiotics to kick the bacteria out. Ignoring it risks letting the infection dig in deeper, potentially causing scarring or even sepsis—a life-threatening spread to your bloodstream. So, don’t roll the dice—see a doctor to get it sorted fast.
- Why do women get kidney infections more often than men?
Blame anatomy for this one! Women have a shorter urethra—the tube that carries urine out of the body—which is like a quick highway for bacteria to reach the bladder and beyond. It’s only about 1.5 inches long in women, compared to 8 inches in men. Plus, the urethra’s closeness to the anus in women makes it easier for bacteria to hop over. Hormonal shifts and pregnancy can also up the odds, making women frequent targets of this pesky infection.
- How painful is a kidney infection?
Picture a deep, nagging ache in your lower back or side, right where your kidneys sit. That’s the signature pain of a kidney infection, and it can range from a dull throb to a sharp stab. Add in burning when you pee, and it’s no picnic. For some, it’s mild enough to shrug off at first, but for others, it’s intense enough to send them straight to bed—or the ER. The good news? Pain relief and treatment can turn down the volume on this discomfort fast.
- Can kids get kidney infections too?
Absolutely, and it’s trickier because kids don’t always complain clearly. Bacteria can invade their little kidneys just like adults’, often from an untreated UTI or a condition where urine flows backward (vesicoureteral reflux). Instead of saying “my back hurts,” they might just be cranky, feverish, or off their food. Parents and doctors need to play detective to catch it early, since kids’ smaller bodies can escalate to complications quicker than adults.
- How does a urinary tract infection (UTI) differ from a kidney infection?
Think of a UTI as the umbrella term—it’s any infection in your urinary system, from the urethra to the kidneys. A kidney infection is a specific, more serious type of UTI that’s climbed the ladder to your kidneys. A basic UTI might just irritate your bladder, causing frequent bathroom trips and burning. But when it hits the kidneys, you’re looking at fever, chills, and back pain—signs the stakes have risen. It’s like the difference between a drizzle and a thunderstorm!
- How much time is needed to heal from a kidney infection?
Recovery’s a bit like a road trip—it depends on how fast you start and the route you take. With antibiotics, most people feel better in 2-3 days, but the full course (usually 7-14 days) is key to wiping out the infection. If it’s severe enough for a hospital stay, add a few extra days for IV treatment and rest. Lingering tiredness might tag along for a week or two, but stick to the plan, and you’ll be back to your old self soon.
- Can a kidney infection cause permanent damage?
Yes, but it’s not a given—it’s more like a warning sign to act fast. If the infection lingers or keeps coming back, it can scar your kidneys, making them less efficient over time. In rare cases, it might lead to chronic kidney disease, where they struggle to filter waste permanently. Kids and people with blockages (like kidney stones) are at higher risk. The silver lining? Quick treatment usually keeps your kidneys in fighting shape.
- Are there natural ways to help a kidney infection?
Nature can lend a hand, but it’s not the whole fix. Drinking tons of water flushes bacteria out, while unsweetened cranberry juice might stop them from clinging to your urinary tract. A heating pad can ease that achy back, and probiotics could balance your body’s good bacteria. But here’s the catch—these are sidekicks, not superheroes. Antibiotics are the real MVPs for clearing the infection, so pair these tricks with a doctor’s advice, not instead of it.
- How can I tell if my kidney infection is getting worse?
Keep an eye out for red flags: a fever that spikes past 102°F (39°C), shaking chills, confusion, or pain that won’t quit even with meds. Vomiting so much you can’t keep fluids down or urine that’s barely trickling out are big clues too. These scream that the infection might be spreading—maybe even to your blood (hello, sepsis). If you spot these, don’t wait—get to a doctor or ER pronto, because time’s ticking when it gets this serious.