Urinary incontinence, a widespread but frequently misunderstood issue, impacts countless individuals across the globe. It refers to the unintentional leakage of urine, which can range from occasional mild leaks to a complete inability to control urination. While it’s more prevalent among older adults, urinary incontinence can affect individuals of any age or gender. The condition can be embarrassing and impact one’s quality of life, but the good news is that it’s often treatable. In this blog post, we’ll explore the types of urinary incontinence, causes of urinary incontinence, symptoms of urinary incontinence, and treatment of urinary incontinence to help you better understand and manage this condition.
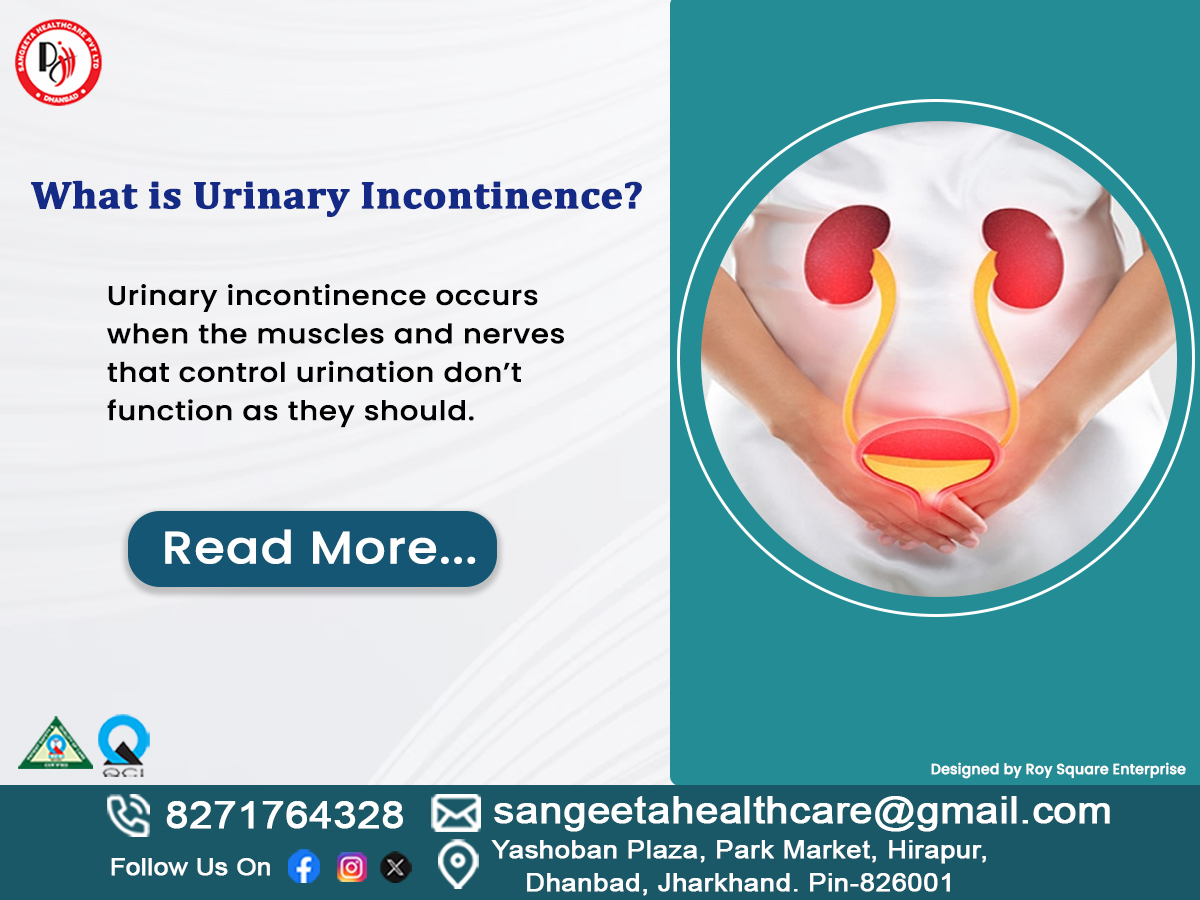
What is Urinary Incontinence?
Urinary incontinence occurs when the muscles and nerves that control urination don’t function as they should. This can lead to accidental urine leakage during everyday activities like coughing, sneezing, laughing, or even exercising. While it’s not a life-threatening condition, it can significantly affect emotional well-being, social interactions, and overall quality of life.
Understanding the different types of urinary incontinence, their causes, and symptoms is the first step toward finding effective treatment options. Let’s break it down.
Types of Urinary Incontinence
Urinary incontinence manifests in various forms, each distinguished by its specific features and causes. Identifying the type you’re experiencing is crucial for proper diagnosis and treatment.
1. Stress Incontinence
Stress incontinence occurs when physical activities or movements put pressure on the bladder, causing urine leakage. Common triggers include coughing, sneezing, laughing, lifting heavy objects, or exercising. This type is more common in women, especially after childbirth or menopause, due to weakened pelvic floor muscles.
-
Urge Incontinence
Urge incontinence, often referred to as “overactive bladder,” involves a sudden and overwhelming need to urinate, which can result in unintentional urine leakage. People with this condition often feel the need to urinate frequently, even at night. It can be caused by nerve damage, infections, or neurological conditions like Parkinson’s disease.
-
Overflow Incontinence
Overflow incontinence happens when the bladder doesn’t empty completely, leading to constant dribbling or frequent leakage. This type is often seen in men with prostate issues or individuals with nerve damage that affects bladder function.
-
Functional Incontinence
Functional incontinence occurs when a physical or cognitive impairment prevents a person from reaching the bathroom in time. For example, arthritis or dementia can make it difficult to move quickly or recognize the need to urinate.
-
Mixed Incontinence
As the name suggests, mixed incontinence is a combination of two or more types, most commonly stress and urge incontinence. This type is often seen in older adults.
Causes of Urinary Incontinence
The causes of urinary incontinence vary depending on the type and individual circumstances. Here are some common factors:

– Weak Pelvic Floor Muscles: Pregnancy, childbirth, and menopause can weaken the pelvic floor muscles, leading to stress incontinence.
– Aging: As we age, the bladder muscles may lose strength, and the urethra may become less flexible.
– Nerve Damage: Conditions like diabetes, multiple sclerosis, or spinal cord injuries can interfere with nerve signals that control bladder function.
– Prostate Issues: In men, an enlarged prostate or prostate surgery can contribute to incontinence.
– Urinary Tract Infections (UTIs): Infections can irritate the bladder, causing temporary incontinence.
– Lifestyle Factors: Factors such as obesity, smoking, and high intake of caffeine or alcohol may elevate the likelihood of developing incontinence.
– Medications: Certain medications, such as diuretics or sedatives, can affect bladder control.
Symptoms of Urinary Incontinence
The symptoms of urinary incontinence depend on the type and severity of the condition. Common signs include:
– Leaking urine during physical activities (stress incontinence).
– Sudden, intense urges to urinate that are difficult to control (urge incontinence).
– Frequent urination, especially at night.
– Dribbling urine or a constant feeling of a full bladder (overflow incontinence).
– Difficulty reaching the bathroom in time due to physical or cognitive limitations (functional incontinence).
If you notice any of these symptoms, it’s crucial to seek advice from a medical professional to obtain an accurate diagnosis and appropriate treatment.
Treatment of Urinary Incontinence
The positive aspect is that urinary incontinence can frequently be managed or cured with proper treatment. The approach to managing urinary incontinence varies based on its type, severity, and the root causes involved. Here are some common approaches:

-
Lifestyle Changes
– Weight Management: losing extra weight can alleviate pressure on the bladder.
– Dietary Adjustments: Avoiding caffeine, alcohol, and spicy foods can help minimize bladder irritation.
– Fluid Management: Drinking the right amount of water (not too much or too little) can improve bladder control.
-
Pelvic Floor Exercises
Kegel exercises are highly effective for strengthening the pelvic floor muscles, especially for stress incontinence. These exercises focus on tightening and releasing the muscles responsible for regulating urination.
-
Medications
Certain medications can help relax the bladder muscles, reduce over activity, or treat underlying conditions like UTIs.
-
Medical Devices
For women, devices like pessaries can support the bladder and reduce leakage. In some cases, a urethral insert may be used to block urine flow during physical activities.
-
Behavioral Therapies
Bladder training techniques, such as scheduled bathroom visits and delayed urination, can help improve bladder control over time.
-
Surgical Options
For severe cases, surgical procedures like sling surgery or bladder neck suspension may be recommended to provide additional support to the bladder or urethra.
-
Alternative Therapies
Acupuncture, biofeedback, and electrical stimulation are alternative treatments that some people find helpful.
When to See a Doctor
If urinary incontinence is affecting your daily life, don’t hesitate to seek medical advice. Detecting and addressing the issue early can help stop it from getting worse and enhance your overall well-being. Your doctor may perform a physical exam, urine tests, or bladder function tests to determine the cause and recommend the best treatment plan.
Final Thoughts
Urinary incontinence is a common condition that can be managed effectively with the right approach. By understanding the types of urinary incontinence, causes of urinary incontinence, symptoms of urinary incontinence, and treatment of urinary incontinence, you can take proactive steps toward better bladder health. Remember, you’re not alone, and help is available. Don’t let embarrassment prevent you from seeking the care you deserve.
If you or a loved one is experiencing symptoms of urinary incontinence, consult a healthcare professional to explore treatment options tailored to your needs. With the right support, you can regain control and live a confident, active life.
Here are some FAQs :
- What is urinary incontinence?
Urinary incontinence refers to the involuntary release of urine caused by an inability to control the bladder. It can range from mild leaks to complete loss of control and affects people of all ages.
- Mention different types of urinary incontinence.
The main types are:
– Stress Incontinence: Involuntary loss of urine can occur during actions such as coughing or sneezing.
– Urge Incontinence: Experiencing sudden and overwhelming urges to urinate can be disruptive and concerning.
– Overflow Incontinence: Constant dribbling from an overfull bladder.
– Functional Incontinence: Difficulty in reaching the restroom promptly.
– Mixed Incontinence: A mix of stress and urge incontinence can occur when both types of urinary incontinence are present simultaneously.
- What causes urinary incontinence?
Common causes include weak pelvic muscles, nerve damage, prostate issues, UTIs, obesity, and certain medications.
- Does urinary incontinence naturally occur as a person gets older?
No, it’s not inevitable. Although it is more frequently observed in older individuals, the condition is typically treatable and should not be considered an inevitable aspect of aging.
- Can urinary incontinence be cured?
Numerous cases can be effectively managed or resolved through treatments such as pelvic exercises, lifestyle adjustments, medications, or surgical interventions, depending on the underlying cause.
- What are home remedies for managing urinary incontinence?
– Do Kegel exercises.
– Avoid caffeine, alcohol, and spicy foods.
– Maintain a healthy weight.
– Use absorbent pads if needed.
– Schedule regular bathroom visits.
- When should I consult a doctor for urinary incontinence?
See a doctor if:
– It affects your daily life.
– You have pain, blood in urine, or frequent UTIs.
– Home remedies don’t help.
- Can men experience urinary incontinence?
Men can also encounter this condition, frequently as a result of prostate-related problems or surgical procedures. Overflow incontinence is most common.
- Are there any medications for urinary incontinence?
Certain medications, such as anticholinergics or beta-3 agonists, may be effective in providing relief. Always consult a doctor before starting any treatment.
- Can lifestyle changes really help with urinary incontinence?
Yes! Adopting a healthier diet, managing fluid intake, and losing weight can lead to a notable reduction in symptoms.