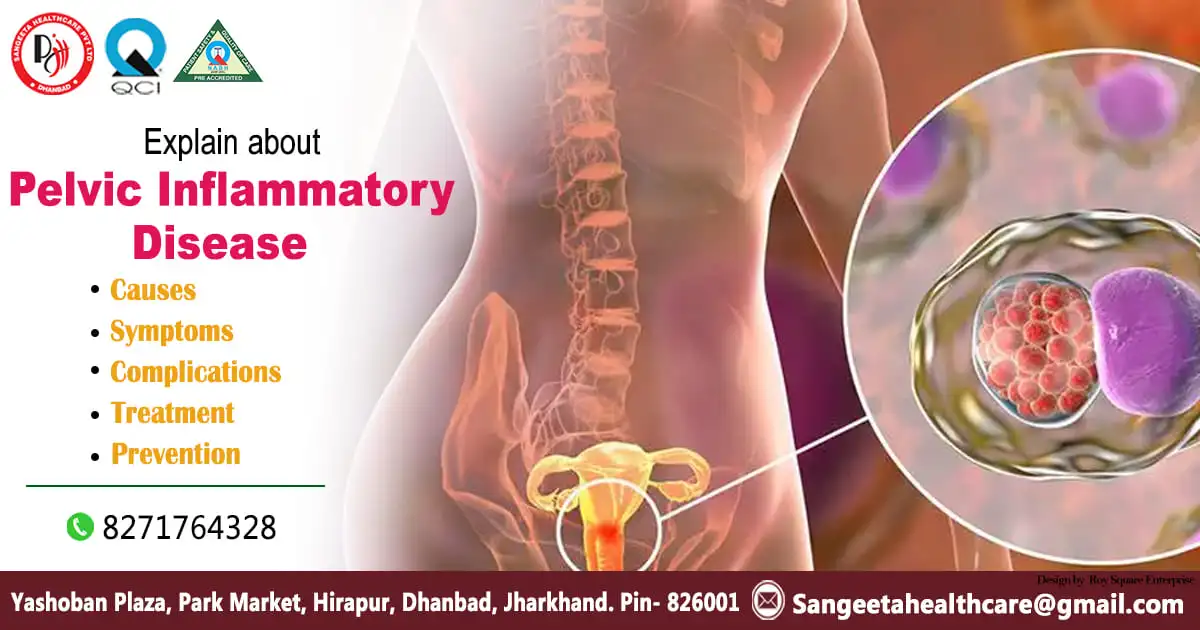
Pelvic Inflammatory Disease

Pelvic Inflammatory Disease (PID) is a serious health condition that affects the female reproductive system. It occurs when bacteria from the vagina or cervix travel upwards into the uterus, fallopian tubes, or ovaries, causing inflammation and infection. PID can have severe consequences if left untreated, including infertility, chronic pelvic pain, and an increased risk of ectopic pregnancy. In this blog post, we will explore the causes, symptoms, and treatment options for Pelvic Inflammatory Disease.
Causes:
The primary cause of PID is the introduction of bacteria into the upper genital tract. The most common bacteria responsible for PID are sexually transmitted infections (STIs), such as Chlamydia and Gonorrhea. However, other bacteria not related to sexual activity can also contribute to PID. Risk factors for PID include multiple sexual partners, a history of STIs, and the use of intrauterine devices (IUDs) for contraception.
Symptoms:
PID symptoms can vary in severity, and some individuals may experience mild discomfort while others may have more pronounced symptoms. Common signs of PID include:
- Pelvic Pain: Persistent and dull pain in the lower abdomen and pelvic region.
- Abnormal Vaginal Discharge: Unusual discharge that may be yellow or green with a foul odor.
- Painful Urination: Discomfort or pain while urinating.
- Irregular Menstrual Bleeding: Changes in the menstrual cycle, including heavier or more painful periods.
- Fever and Chills: Elevated body temperature and chills, indicating an infection.
It’s important to note that some women with PID may not exhibit any noticeable symptoms, making regular gynecological check-ups crucial for early detection.
Complications:
If left untreated, Pelvic Inflammatory Disease can lead to serious complications, including:
- Infertility: Scar tissue from the inflammation can block the fallopian tubes, preventing the egg from reaching the uterus.
- Chronic Pelvic Pain: Persistent pain in the pelvic region that may last for months or years.
- Ectopic Pregnancy: The risk of an ectopic pregnancy (a pregnancy outside the uterus) is higher for women who have had PID.
Treatment:
Prompt and appropriate treatment is crucial to prevent complications. Treatment typically involves a combination of antibiotics to eliminate the infection. In severe cases or if an abscess has formed, hospitalization may be necessary for intravenous antibiotics and, in some cases, surgical intervention to drain the abscess.
Prevention:
Preventing PID involves practicing safe sex, using barrier methods of contraception, and getting regular screenings for STIs. If diagnosed with an STI, it is essential to complete the prescribed course of antibiotics and inform sexual partners to prevent the spread of infection.
Reproductive Tract Infection (RTI)

When it comes to the health of kidney, RTI is the most common terms that affects the organ irrespective of age and gender.
Understand the term:
A Reproductive Tract Infection (RTI) refers to an infection that affects the reproductive organs and structures in both men and women. These infections can involve various components of the reproductive system, including the uterus, fallopian tubes, ovaries, cervix, vagina in women, and the testes, prostate, and other related structures in men. RTIs can be caused by a variety of microorganisms, including bacteria, viruses, fungi, and parasites.
Classification:
RTIs can be classified into two main categories:
Sexually Transmitted Infections (STIs): These are infections that are primarily transmitted through sexual contact. Common STIs that can affect the reproductive tract include Chlamydia, Gonorrhea, Syphilis, Herpes, and Human Papillomavirus (HPV).
Non-Sexually Transmitted Infections: These infections may occur due to non-sexual factors such as poor hygiene, compromised immune function, or the presence of other medical conditions. Bacterial vaginosis, yeast infections, and urinary tract infections are examples of non-sexually transmitted reproductive tract infections.
Symptoms& Prevention:
The symptoms of RTIs can vary widely depending on the specific infection, its severity, and the affected individual’s gender. Common symptoms may include abnormal vaginal or penile discharge, pain or discomfort during urination, pelvic pain, lower abdominal pain, and changes in menstrual patterns.
It’s crucial to diagnose and treat RTIs promptly to prevent complications such as pelvic inflammatory disease, infertility, ectopic pregnancies, and an increased risk of HIV transmission. Prevention measures include practicing safe sex, maintaining good personal hygiene, regular medical check-ups, and, in the case of STIs, informing and treating sexual partners.
As with any medical concern, individuals experiencing symptoms associated with reproductive tract infections should seek medical attention for an accurate diagnosis and appropriate treatment. Early intervention can help manage these infections effectively and reduce the risk of long-term complications.
Minimal pod fluid
In the realm of medical diagnostics, minimal pod fluid is another term that may surface during various tests, particularly when assessing the health of the kidneys. Understanding what minimal pod fluid entails is crucial for individuals and healthcare providers alike. Nextin this blog post, we’ll explore the concept of minimal pod fluid, its significance, and what it might indicate for your health.
Defining Minimal Pod Fluid:
Minimal pod fluid, also known as minimal change disease (MCD), refers to a kidney condition characterized by abnormal functioning of the glomeruli, the tiny filtering units within the kidneys. In individuals with minimal pod fluid, these glomeruli appear normal under a microscope, and the condition is often diagnosed through a renal biopsy.
Causes:
The exact cause of minimal pod fluid is not always clear, but it is believed to be related to an immune system dysfunction. In some cases, it may be triggered by infections, allergic reactions, or certain medications. Minimal change disease is more commonly observed in children, but it can affect individuals of any age.
Symptoms:
One of the challenging aspects of minimal pod fluid is that it often presents with few or no noticeable symptoms. However, some individuals may experience:
- Swelling (Edema): Swelling, particularly in the legs and around the eyes, may occur due to the retention of fluids.
- Foamy Urine: The presence of excess protein in the urine can result in foamy or bubbly urine.
- Fatigue:It’s possible for some people to feel weak or exhausted.
Diagnosis:
The diagnosis of minimal pod fluid typically involves a combination of medical history, physical examination, and laboratory tests. A renal biopsy is often the definitive method to confirm the presence of minimal change disease and rule out other kidney conditions.
Treatment:
The good news is that minimal pod fluid often responds well to treatment. The primary approach involves the use of corticosteroid medications, which can help reduce inflammation and improve kidney function. In most cases, individuals with minimal change disease have a favourable prognosis, with many achieving complete remission.
While minimal pod fluid might sound concerning, it is important to remember that it is a treatable condition, especially when diagnosed early. Regular check-ups, particularly if you notice any unusual symptoms like swelling or changes in urine, are essential for maintaining kidney health. If you or someone you know is diagnosed with minimal pod fluid, working closely with healthcare providers to develop a personalized treatment plan can lead to successful management and improved long-term outcomes.
Inflammatory Smear:
The realm of women’s health is vast and intricate, with various screenings and tests aimed at maintaining reproductive well-being. One such crucial diagnostic tool is the inflammatory smear, an examination that plays a pivotal role in assessing the health of the female reproductive system. Now, we’ll delve into the significance of inflammatory smears, what they entail, and why they are an essential aspect of women’s healthcare.
Understanding Inflammatory Smear:
An inflammatory smear, commonly known as a Pap smear or Pap test, is a routine screening procedure designed to detect abnormal changes in the cells of the cervix, the lower part of the uterus. The primary goal of this test is to identify early signs of cervical cancer or precancerous conditions, allowing for timely intervention and prevention.
Procedure:
During the inflammatory smear procedure, a healthcare provider collects a small sample of cells from the cervix using a soft brush or spatula. The collected cells are then examined under a microscope to identify any abnormalities, such as changes in size, shape, or organization. This microscopic analysis helps detect potential issues at an early stage when they are more manageable and treatable.
Importance of Inflammatory Smear:

- Early Detection of Cervical Abnormalities: Inflammatory smears are instrumental in identifying abnormal cellular changes in the cervix, which could indicate the presence of human papillomavirus (HPV) or other factors that may lead to cervical cancer.
- Preventing Cervical Cancer: By detecting and addressing abnormalities early, inflammatory smears contribute significantly to preventing the development of cervical cancer. Early intervention can involve monitoring, medical treatments, or minor surgical procedures, depending on the severity of the findings.
- Monitoring Reproductive Health: Inflammatory smears are part of routine gynaecological examinations, allowing healthcare providers to monitor a woman’s reproductive health over time. Regular screenings help track changes, assess risk factors, and tailor preventive measures accordingly.
- HPV Detection: Inflammatory smears also play a crucial role in detecting the presence of HPV, a common sexually transmitted infection linked to cervical cancer. Identifying HPV early enables healthcare providers to monitor and manage the infection effectively.
Inflammatory smears are an indispensable tool in women’s healthcare, contributing to the prevention and early detection of cervical abnormalities. Regular screenings empower women to take charge of their reproductive health, providing a foundation for timely interventions that can ultimately save lives. It’s essential for women to prioritize routine gynaecological check-ups, including inflammatory smears, as part of a proactive approach to overall well-being. Remember, early detection is key, and staying informed about your health is a powerful step towards a healthier future.
In the conclusion of Pelvic Inflammatory Disease, it can be said that it is a serious health concern that requires prompt attention. Understanding the causes, recognizing symptoms, and seeking timely medical intervention are crucial for preventing long-term complications. Regular gynaecological check-ups, open communication with healthcare providers, and practicing safe sex are essential steps in maintaining reproductive health and preventing the occurrence of PID.









 Symptoms:
Symptoms:
