Empower Your Pelvic Health: Rising Stronger from Uterine Prolapse

Uterine Prolapse
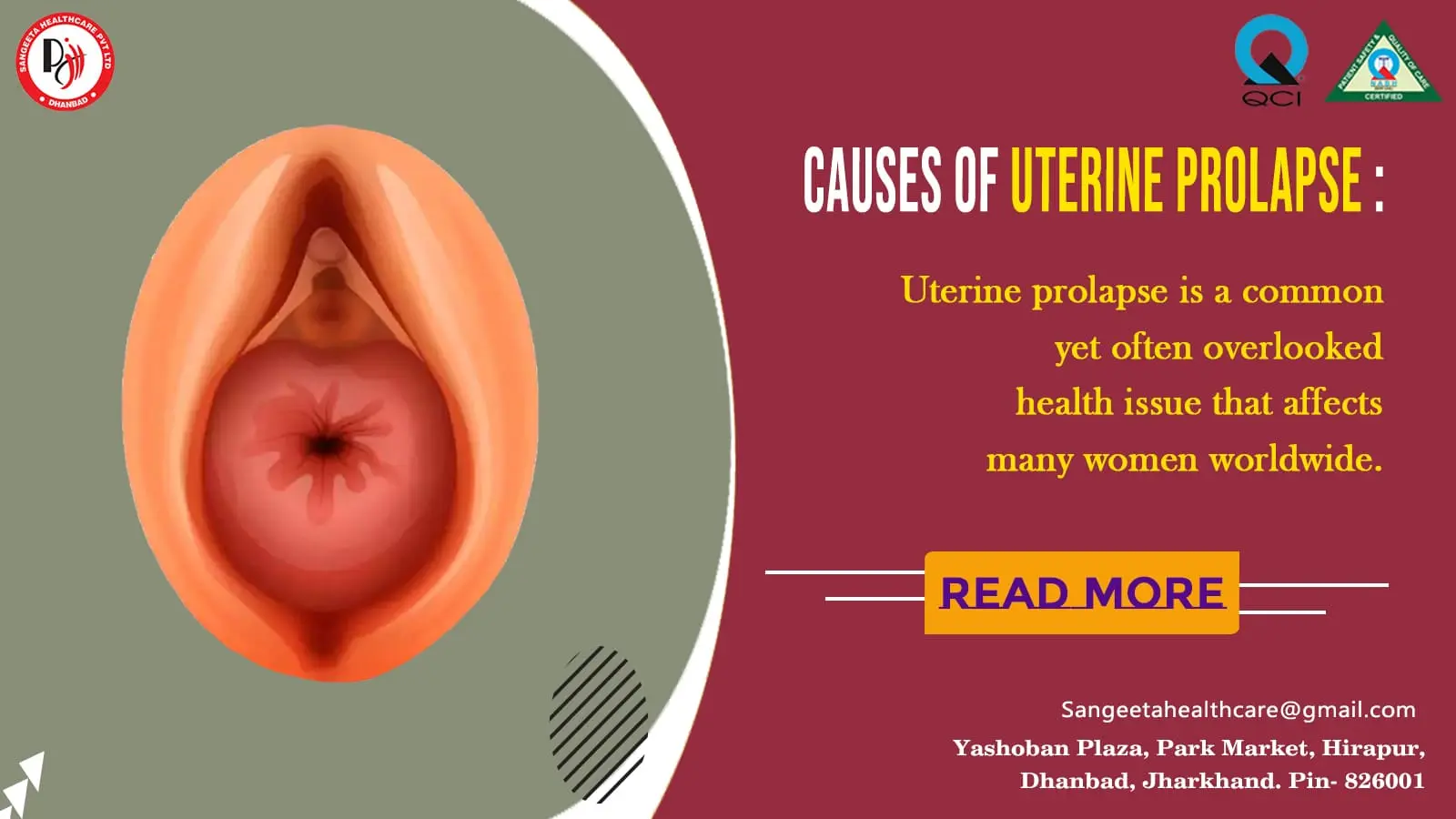
 Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.
Uterine prolapse is a common yet often overlooked health issue that affects many women worldwide. This condition occurs when the pelvic floor muscles and ligaments weaken, leading to the descent of the uterus into the vaginal canal. In this blog, we will delve into the causes, symptoms, and various treatment options for uterine prolapse, shedding light on a topic that is crucial for women’s health.
Causes of Uterine Prolapse:
- Pregnancy and Childbirth: The strain on pelvic muscles during pregnancy and the trauma of childbirth can weaken the supportive tissues of the uterus.
- Aging: As women age, hormonal changes and the natural aging process can contribute to the weakening of pelvic floor muscles.
- Menopause: Reduced estrogen levels after menopause can lead to a loss of muscle tone and contribute to uterine prolapse.
- Hysterectomy: Surgical removal of the uterus can disrupt the supporting structures, increasing the risk of prolapse.
- Obesity and Chronic Constipation: Excessive weight and straining during bowel movements can strain the pelvic floor and contribute to prolapse.
Symptoms of Uterine Prolapse:
- Sensation of a Bulge: Women with uterine prolapse may feel a bulge or pressure in the vaginal area.
- Pelvic Discomfort: Discomfort or pain in the pelvic region, especially when sitting or standing for extended periods.
- Problems with Urination and Bowel Movements: Difficulty emptying the bladder or bowels, frequent urinary tract infections, and urinary incontinence.
- Backache and Lower Abdominal Pain: Pain in the lower back and abdomen may be experienced, particularly during intercourse.
- Vaginal Bleeding or Discharge: Some women may notice spotting or an unusual discharge.
Treatment Options:
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles through exercises can provide support and alleviate mild cases of uterine prolapse.
- Hormone Replacement Therapy (HRT): Estrogen therapy may be recommended for postmenopausal women to improve tissue elasticity and muscle tone.
- Pessary Use: A pessary is a device inserted into the vagina to support the uterus and alleviate symptoms.
- Surgery: In severe cases, surgical interventions like hysterectomy or uterine suspension may be considered to repair and reinforce the pelvic structures.
Prevention and Lifestyle Changes:
1. Maintain a Healthy Weight: Obesity increases the risk of uterine prolapse, so maintaining a healthy weight is crucial.
2. Regular Exercise: Engage in pelvic floor exercises and overall fitness routines to strengthen muscles and maintain a healthy lifestyle.
3. Proper Lifting Techniques: Lift heavy objects using proper techniques to avoid straining the pelvic floor.
Uterine prolapse is a manageable condition with various treatment options available. It is essential for women to be aware of the risk factors, recognize symptoms, and seek timely medical advice. By understanding uterine prolapse, we can empower women to take proactive steps in maintaining their reproductive health and overall well-being.
Uterine prolapse is a condition that can have various implications for a woman’s health, and one of the potential complications associated with it is the development of decubitus ulcers, also known as pressure sores or bedsores. Next, we’ll explore the connection between uterine prolapse and decubitus ulcers, understanding the risk factors, symptoms, prevention, and management strategies.
Understanding Decubitus Ulcers:
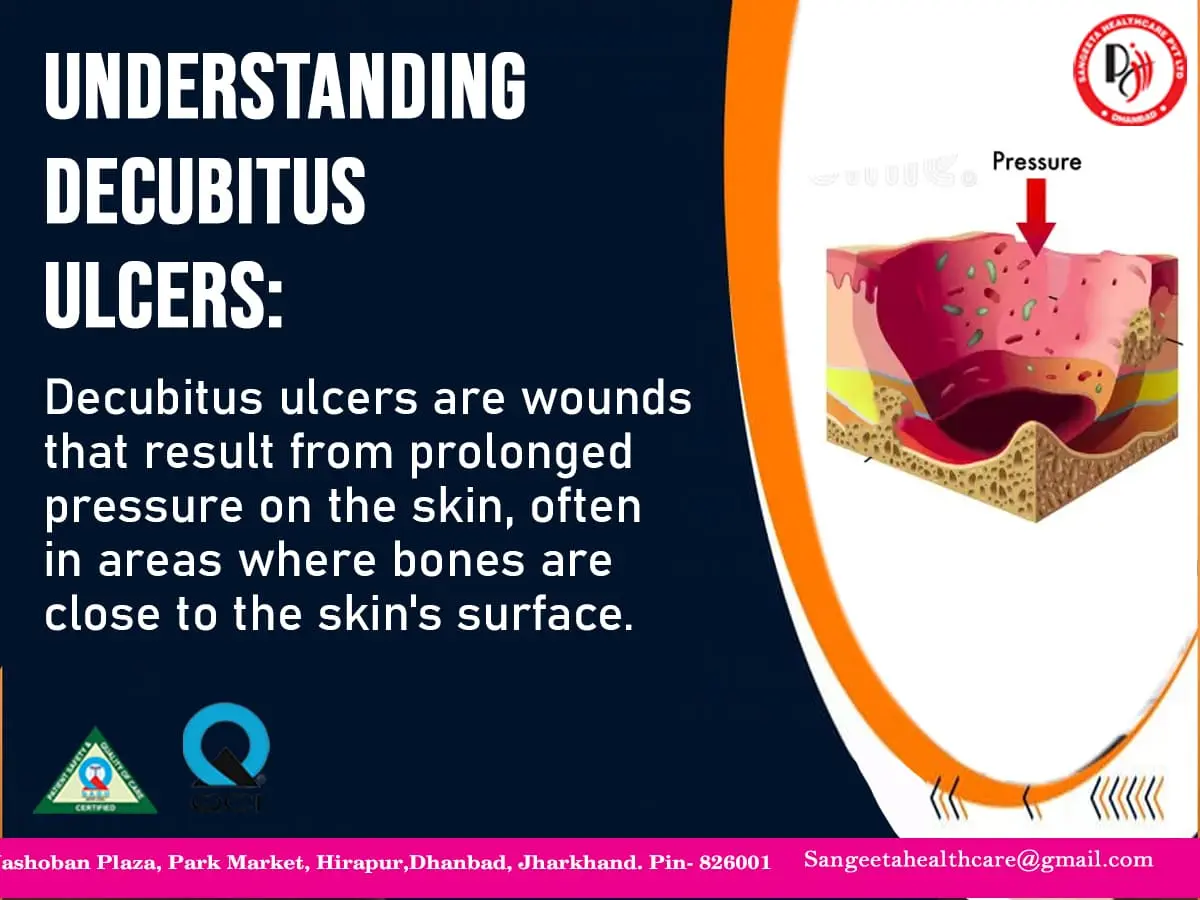
Decubitus ulcers are wounds that result from prolonged pressure on the skin, often in areas where bones are close to the skin’s surface. In the context of uterine prolapse, the pressure from the displaced uterus against the vaginal wall and surrounding tissues can create conditions conducive to the development of these ulcers.
Risk Factors:
- Prolonged Immobility: Women with uterine prolapse may experience discomfort or pain, leading to reduced mobility, especially if the condition is severe.
- Poor Circulation: The pressure exerted by the prolapsed uterus can impede blood flow to specific areas, increasing the risk of tissue damage.
- Incontinence: Urinary or fecal incontinence, common in uterine prolapse, can contribute to moisture on the skin, making it more susceptible to breakdown.
- Poor Nutrition: Inadequate nutrition can compromise the skin’s integrity, making it more prone to developing ulcers.
Symptoms of Decubitus Ulcers:
- Skin Discoloration: Changes in skin color, ranging from red to purple, may be observed.
- Swelling and Tenderness: The affected area may become swollen, and the skin may be tender to the touch.
- Open Sores or Blisters: As the condition progresses, open sores or blisters may develop, exposing underlying tissues.
- Pus or Drainage: Infected ulcers may produce pus or other types of drainage.
- Foul Odor: Infections associated with decubitus ulcers can cause a foul odor.
Prevention Strategies:
1. Regular Position Changes: Encourage women with uterine prolapse to change positions frequently to alleviate pressure on vulnerable areas.
2. Use of Supportive Devices: Employing cushions or pillows to support the pelvic region can help distribute pressure more evenly.
3. Maintain Good Hygiene: Regular cleansing and proper care of the perineal area can prevent infections and minimize the risk of ulcers.
4. Nutritional Support: Ensure a well-balanced diet rich in nutrients to promote overall skin health.
5. Seek Prompt Medical Attention: Address any signs of skin breakdown or infection promptly to prevent complications.
Management of Decubitus Ulcers:
- Wound Care: Keep the ulcer clean and apply appropriate dressings to promote healing.
- Infection Control: Administer antibiotics if there is evidence of infection.
- Offloading Pressure: Utilize pressure-relieving devices and techniques to reduce further pressure on affected areas.
- Pain Management: Address pain associated with ulcers through medications or alternative pain management strategies.
Understanding the potential risk of decubitus ulcers in the context of uterine prolapse is crucial for both healthcare providers and women themselves. By adopting preventive measures and seeking prompt medical attention, we can minimize the impact of these complications and work towards ensuring the overall well-being of women experiencing uterine prolapse.
Complete procidentia, a severe form of uterine prolapse, poses unique challenges to women’s health, often involving the protrusion of the entire uterus through the vaginal opening. Now, explore the intricacies of complete procidentia and delve into the associated issue of uterine over-distension, shedding light on the causes, symptoms, and potential treatment options.
Understanding Complete Procidentia:
Complete procidentia is an advanced stage of uterine prolapse where the uterus descends entirely into or beyond the vaginal opening. This condition is often characterized by significant discomfort, pain, and a noticeable bulge, impacting a woman’s quality of life and daily activities.
Causes of Complete Procidentia:
- Weakened Pelvic Floor Muscles: Prolonged weakening of the pelvic floor muscles, often due to factors like childbirth, aging, or hormonal changes, can contribute to the severity of uterine prolapse.
- Multiple Vaginal Deliveries: Women who have undergone multiple vaginal deliveries face an increased risk of complete procidentia.
- Hysterectomy Complications: Surgical removal of the uterus (hysterectomy) can sometimes lead to inadequate support of the pelvic structures, increasing the likelihood of prolapse.
- Connective Tissue Disorders: Conditions affecting the connective tissues, such as Ehlers-Danlos syndrome, can predispose individuals to uterine prolapse.
Consequences of Uterine Over-Distension:
1. Increased Discomfort and Pain: As the uterus protrudes, it can cause heightened discomfort, pain, and pressure in the pelvic region.
2. Urinary and Fecal Incontinence: Over-distension of the uterus may compromise the integrity of the surrounding structures, leading to issues with bladder and bowel control.
3. Difficulty with Daily Activities: Women with complete procidentia may find it challenging to engage in routine activities such as walking, standing, or even sitting comfortably.
4. Psychological Impact: The physical and emotional toll of complete procidentia can contribute to psychological distress, affecting a woman’s self-esteem and mental well-being.
Treatment Options:
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles can provide support and alleviate mild symptoms.
- Pessary Use: A pessary, a device inserted into the vagina to support the uterus, may be recommended to manage symptoms.
- Hormone Replacement Therapy (HRT): Estrogen therapy can help improve tissue elasticity and muscle tone, particularly in postmenopausal women.
- Surgical Intervention: In severe cases, surgery may be required to repair and reinforce the pelvic structures, possibly involving a hysterectomy.
Lifestyle Changes and Coping Strategies:
- Maintain a Healthy Weight: Obesity can exacerbate uterine prolapse, so maintaining a healthy weight is essential.
- Avoid Heavy Lifting: Minimize activities that involve heavy lifting to reduce strain on the pelvic floor.
- Regular Medical Check-ups: Routine gynecological examinations can help detect and address uterine prolapse at an early stage.
Complete procidentia, coupled with uterine over-distension, demands careful attention and comprehensive management. By understanding the causes, symptoms, and available treatment options, women and healthcare providers can work together to address the challenges posed by this complex condition and improve the overall well-being of those affected. Early intervention and a holistic approach are key to managing complete procidentia and mitigating its impact on women’s lives.


